Gastroesophageal reflux disease (GERD) is an incredibly common condition affecting millions worldwide. Characterized by persistent heartburn, regurgitation, and sometimes even difficulty swallowing, it’s often dismissed as merely a bothersome digestive issue. However, GERD can have far-reaching effects on the body, potentially extending beyond the esophagus and into areas seemingly unrelated to digestion. This is where questions arise about connections between GERD symptoms and other bodily changes, such as swollen lymph nodes – a sign that often triggers concern due to its association with illness and infection. Understanding whether these two are linked requires delving into the complex interplay of the digestive system, the immune response, and potential underlying causes.
The feeling of something being “off” when experiencing GERD can be unsettling, leading individuals to search for explanations beyond the typical acid reflux symptoms. Swollen lymph nodes, often discovered during self-examination or a routine checkup, are naturally interpreted as indicators of infection or more serious illness. This leads many to wonder if their GERD is somehow causing the swollen nodes, or whether there’s a shared underlying factor contributing to both. The relationship isn’t always straightforward, and it’s crucial to approach this concern with accurate information and, importantly, guidance from a healthcare professional. It’s essential to remember that correlation doesn’t equal causation, and many other conditions can cause swollen lymph nodes independent of digestive issues.
Understanding the Connection: Inflammation & Immune Response
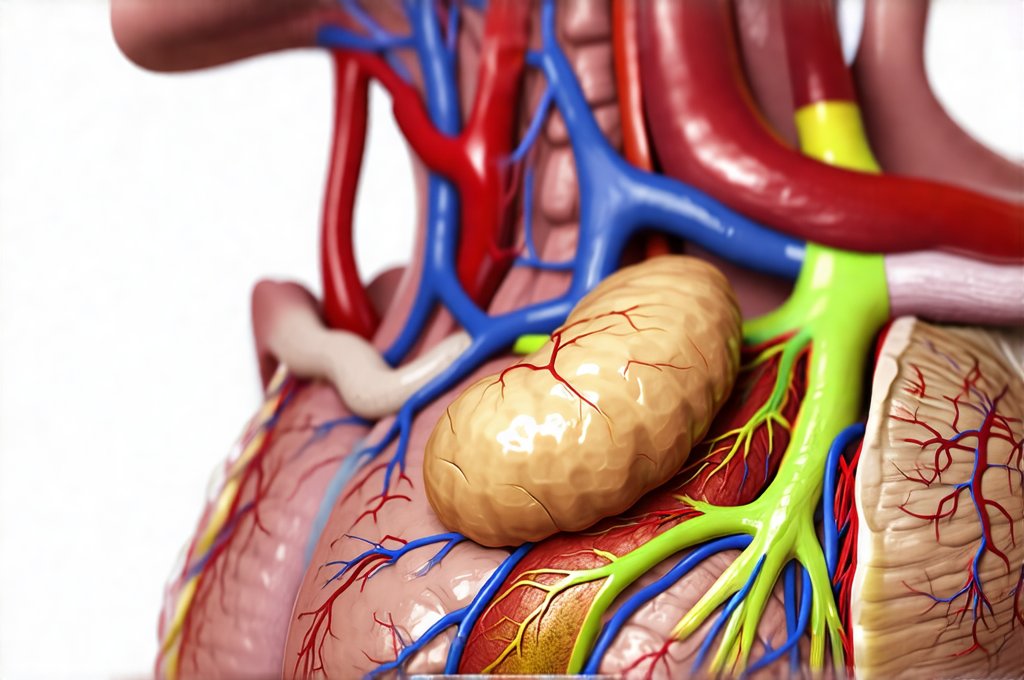
The link between GERD and swollen lymph nodes isn’t necessarily direct in most cases, but it stems from the body’s natural inflammatory response. Chronic acid reflux, a hallmark of GERD, irritates the esophageal lining. This persistent irritation triggers an inflammatory cascade within the body as the immune system attempts to heal the damaged tissue. While inflammation is vital for healing, chronic or prolonged inflammation can sometimes lead to systemic effects—meaning it impacts areas beyond just the esophagus. Lymph nodes are integral parts of the immune system; they filter lymph fluid and house white blood cells that fight off infection. When inflammation occurs elsewhere in the body, the lymphatic system can become activated, potentially leading to swollen lymph nodes in nearby regions.
The location of the swollen lymph nodes is also significant. While GERD itself doesn’t typically cause widespread lymph node swelling, it could theoretically contribute to inflammation in areas close to the esophagus and upper digestive tract. This might result in palpable (detectable by touch) lymph nodes in the neck or collarbone region. However, this is less common than swollen nodes appearing due to more typical causes like viral infections or bacterial illnesses. It’s important to note that GERD-related inflammation isn’t usually strong enough to cause significant or persistent swelling on its own; it’s often a contributing factor rather than the primary driver.
Furthermore, some individuals with GERD may experience microscopic esophagitis, even without noticeable symptoms beyond mild discomfort. This low-grade inflammation can still activate the immune system and contribute to subtle lymphatic responses. The body is constantly working to maintain balance (homeostasis), and any disruption – like chronic acid exposure – will prompt an immune response, even if it’s not immediately apparent as a severe illness. Understanding inflammation is key to understanding these connections.
Potential Complications & Underlying Causes
GERD can sometimes lead to more significant complications that could indirectly contribute to swollen lymph nodes. One such complication is Barrett’s esophagus, a condition where the normal lining of the esophagus changes due to chronic acid exposure. Barrett’s esophagus increases the risk of esophageal cancer, although this is relatively rare. If cancer develops (even in its early stages), it can directly cause regional lymph node swelling as cancerous cells spread and the immune system attempts to fight them off. This is why any persistent or unexplained swollen lymph nodes warrant medical evaluation, even if you have GERD.
Another less common complication is esophageal stricture – a narrowing of the esophagus caused by scarring from chronic inflammation. While not directly causing lymph node swelling, the difficulty swallowing associated with strictures can lead to changes in dietary habits and potentially malnutrition. A weakened immune system due to poor nutrition could make an individual more susceptible to infections that do cause swollen lymph nodes. It’s vital to recognize this indirect link: GERD doesn’t directly cause infection, but it might create conditions where the body is less able to fight one off effectively. Consider if elimination diets could help manage underlying sensitivities.
Finally, there are underlying causes of both GERD and swollen lymph nodes that may overlap. For example, certain autoimmune disorders can manifest as both digestive issues (like reflux) and immune system dysregulation (leading to lymph node swelling). Conditions like Sjogren’s syndrome or systemic lupus erythematosus can affect multiple body systems, creating a complex clinical picture where GERD and swollen nodes coexist but aren’t directly causally linked. If you suspect your GERD is related to other issues, an at-home gut health test could provide valuable insight.
When to Seek Medical Attention & Diagnostic Approaches
Determining the cause of swollen lymph nodes is crucial, especially when accompanied by GERD symptoms. Don’t self-diagnose. Here are some key indicators that warrant a visit to your doctor:
- Swollen lymph nodes that are large (greater than 1 cm in diameter).
- Nodes that feel hard or fixed in place (not movable).
- Nodes accompanied by fever, night sweats, unexplained weight loss, or fatigue.
- Nodes that persist for more than a few weeks without improvement.
Your healthcare provider will likely begin with a thorough physical examination and review of your medical history. Diagnostic tests may include:
- Blood Tests: To assess your overall health, check for signs of infection, inflammation, or autoimmune disorders.
- Imaging Studies: Such as ultrasound, CT scan, or MRI, to visualize the lymph nodes and surrounding tissues. These can help determine their size, shape, and whether there are any concerning features.
- Endoscopy: If GERD is suspected to be contributing to inflammation, an endoscopy might be performed to examine the esophagus and stomach for signs of damage or Barrett’s esophagus.
- Lymph Node Biopsy: In some cases, a biopsy may be necessary to determine the exact cause of the swollen lymph nodes – especially if cancer is suspected.
It’s important to communicate your GERD symptoms clearly to your doctor, even if you don’t think they are related to the lymph node swelling. Providing a complete picture of your health will help them make an accurate diagnosis and recommend the appropriate treatment plan. Remember, proactive healthcare is key – early detection and intervention are always preferable to delaying medical attention. If GERD is causing significant discomfort, understanding GERD with esophagitis or GERD without esophagitis can help you discuss treatment options with your doctor. Finally, be aware of the symptoms related to colon polyps as well.