Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide, often manifesting as heartburn or acid indigestion. However, its reach extends far beyond these typical symptoms, sometimes presenting in unexpected ways that can be deeply unsettling for those experiencing them. Many individuals report sudden urges to stretch, seemingly out of nowhere, or an abrupt need to gasp for air, even when not physically exerting themselves. These aren’t necessarily signs of a cardiac or respiratory issue; they can, and frequently are, directly linked to GERD and the complex interplay between the digestive system, the vagus nerve, and the body’s natural stress response. Understanding this connection is crucial for accurate diagnosis and effective management. Considering your overall diet may also help, so take a look at gerd diet.
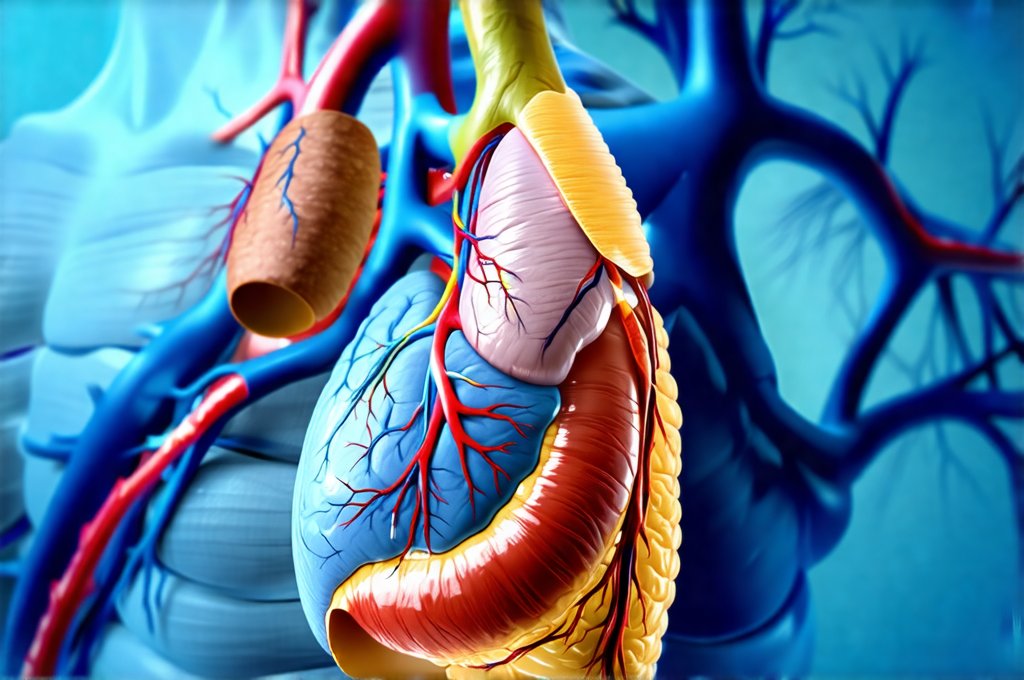
The link isn’t always immediately obvious because these symptoms appear seemingly unrelated to typical heartburn. The esophagus, when irritated by stomach acid repeatedly flowing upwards, can trigger a cascade of neurological responses. This irritation often stimulates the vagus nerve – a long cranial nerve running from the brainstem down to the abdomen – which plays a key role in regulating numerous bodily functions including heart rate, breathing, and digestion. When this nerve is overstimulated due to esophageal inflammation, it can send signals that are misinterpreted by the brain as something requiring immediate physical response, like needing more air or stretching to relieve discomfort. This often leads individuals to attribute these sensations to other causes, delaying appropriate evaluation for GERD. You may also want to learn more about understanding esophagitis and its relation to this condition.
The Vagus Nerve and Reflux: A Complex Connection
The vagus nerve is at the heart of this connection between GERD symptoms and seemingly unrelated physical responses. It’s a bidirectional communication highway; it receives information from the gut and sends signals to it, as well as to other vital organs. In the context of GERD, chronic acid exposure inflames the esophageal lining. This inflammation isn’t simply localized pain; it generates nerve impulses that travel along the vagus nerve. These impulses can be perceived in several ways: as chest pain mimicking cardiac issues, as a tightening sensation in the throat, or even as shortness of breath and the urgent need to gasp for air. The brain, receiving these signals, struggles to pinpoint their origin accurately, often leading to misinterpretations. If you suspect GERD with esophagitis, consider checking out k21.0 gerd.
This vagal stimulation also explains the sudden urge to stretch. When the esophagus is irritated and inflamed, the muscles surrounding it can spasm. This muscle activity, coupled with the neurological signals sent via the vagus nerve, can create a sensation of tightness or constriction in the chest and upper back. The body’s natural response to this perceived restriction is often to attempt to relieve the pressure by stretching – hence the sudden, unexplained urge to extend and lengthen muscles. It’s essentially an instinctive attempt to physically counteract what the brain perceives as a physical limitation, even though the root cause isn’t muscular but rather esophageal irritation.
Furthermore, the vagus nerve’s involvement can contribute to increased anxiety around breathing. The sensation of not getting enough air, even if objectively there is sufficient oxygen intake, creates a feedback loop. Anxiety exacerbates the feeling of breathlessness, leading to hyperventilation and further reinforcing the perceived need to gasp for air. This cycle can be particularly distressing and lead people to worry about underlying respiratory or cardiac problems when GERD is the primary driver.
Why Stretching Feels Necessary
The stretching impulse isn’t simply a random occurrence; it has roots in physiological mechanisms designed to protect us. When we experience discomfort, our bodies instinctively try to alleviate it. In this case, the perceived discomfort from esophageal inflammation triggers a neurological response that prompts muscle lengthening and extension. This is partly due to the way pain signals are processed – the brain often attempts to find ways to physically resolve or diminish the source of pain.
- Stretching can temporarily distract from the underlying discomfort in the esophagus.
- It provides a sense of control, even if it doesn’t actually address the GERD itself.
- The act of stretching releases endorphins, which are natural mood boosters and can offer temporary relief from anxiety associated with the symptoms.
It’s important to recognize that this is a compensatory mechanism, not a solution. While stretching may provide fleeting relief, it doesn’t address the underlying issue of acid reflux. Repeatedly relying on stretching as a coping strategy can mask the GERD and delay appropriate treatment. The constant need to stretch also contributes to muscle fatigue and potential discomfort in other areas of the body, creating a vicious cycle. To better manage your diet related to this condition, consider dinner meals.
Breathlessness and Reflux: A Dangerous Misinterpretation
The sensation of breathlessness associated with GERD isn’t typically caused by actual obstruction of the airways. Instead, it’s usually due to vagal nerve stimulation impacting the respiratory center in the brain. The inflamed esophagus sends signals that are misinterpreted as a lack of oxygen or an inability to breathe effectively, prompting the urgent need to gasp for air. This can be incredibly frightening, leading individuals to fear they’re having a panic attack or experiencing a serious cardiovascular event.
The key difference between GERD-related breathlessness and other causes is that it often occurs without any objective signs of respiratory distress – normal oxygen saturation levels, no wheezing or labored breathing sounds. It’s a neurological phenomenon driven by misinterpretation rather than physical obstruction. However, this can be difficult to discern without proper medical evaluation. If you are reacting to something and unsure what, consider food or environment.
Differentiating from Other Conditions
It’s crucial to differentiate these symptoms from other conditions that can cause similar sensations. Heart disease, asthma, and anxiety disorders all present with breathlessness or chest discomfort. A thorough medical evaluation is necessary to rule out these possibilities before attributing the symptoms solely to GERD. This evaluation typically includes:
- Physical exam
- Review of medical history
- Diagnostic tests such as ECG (electrocardiogram), pulmonary function tests, and potentially an endoscopy to directly visualize the esophagus.
Never self-diagnose. If you’re experiencing sudden urges to stretch or gasp for air, particularly if they are accompanied by chest pain, seek medical attention promptly. While GERD can often be managed with lifestyle changes and medication, it’s essential to rule out more serious conditions first. The goal is accurate diagnosis and a tailored treatment plan that addresses the underlying cause of your symptoms. Before any procedures like colonoscopies, proper preparation is key to ensure accuracy.