Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide, often characterized by frequent heartburn and acid regurgitation. While many associate GERD primarily with these digestive symptoms, its impact can extend beyond the esophagus, sometimes manifesting in less understood ways such as spasms or discomfort in the diaphragm area. These spasms aren’t typically part of the ‘classic’ GERD presentation, leading to confusion and concern for those experiencing them. Understanding the potential link between GERD and diaphragmatic spasms requires delving into the complex interplay between the digestive system, the nerves controlling breathing, and how chronic acid exposure can sometimes disrupt these delicate mechanisms.
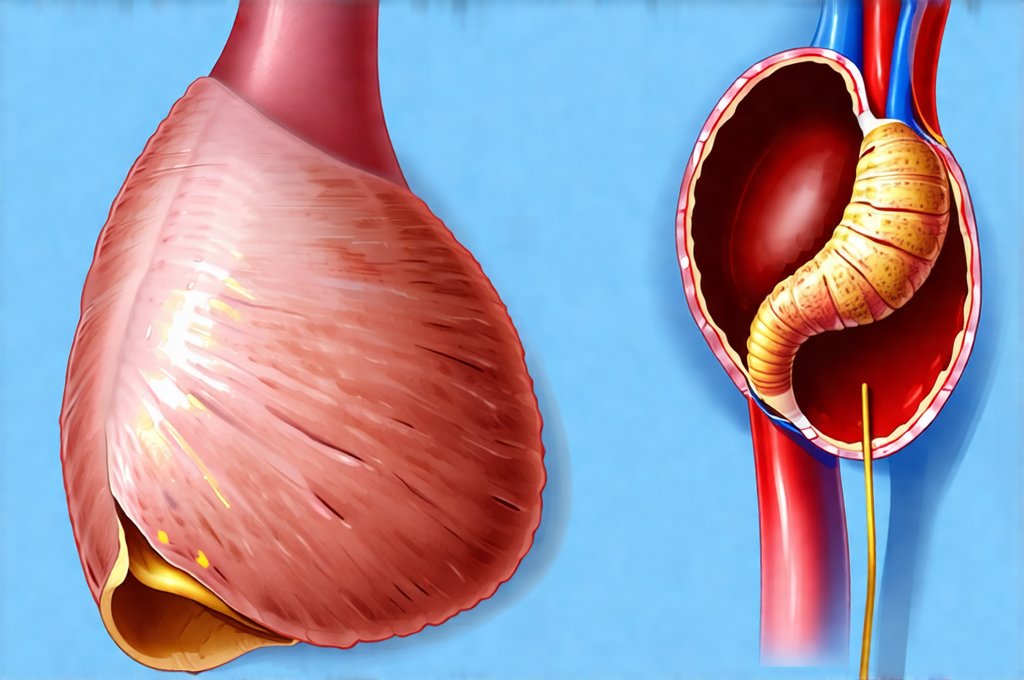
The diaphragm, a large dome-shaped muscle at the base of the chest cavity, plays a vital role in respiration – essentially, it’s what allows us to breathe. It also has important connections with the esophagus and stomach. GERD creates an inflammatory environment that can impact surrounding tissues, potentially affecting nerve pathways or directly irritating the diaphragm itself. Diaphragmatic spasms feel like sudden, involuntary contractions of the muscle, often described as a tightening or cramping sensation in the chest or abdomen. While often benign and temporary, they can be alarming, especially when occurring alongside GERD symptoms or feeling particularly intense. This article will explore the possible connections between these two conditions, potential causes, ways to manage the discomfort, and when it’s important to seek medical attention.
The Connection Between GERD and Diaphragmatic Spasms
The relationship between GERD and diaphragmatic spasms isn’t fully understood, and research continues to investigate the intricacies of this connection. It is not a direct causal link in most cases; rather, it’s often a complex interplay of factors. Chronic acid reflux can lead to inflammation not only in the esophagus but also in surrounding areas, including the nerves that innervate the diaphragm. This inflammatory process may disrupt normal nerve function and increase sensitivity, making the diaphragm more prone to spasms. Essentially, the persistent irritation from GERD could lower the threshold for diaphragmatic muscle contractions.
Another potential mechanism involves the phrenic nerve, which controls the diaphragm’s movement. The phrenic nerve originates in the neck and travels down to the diaphragm; its pathway can sometimes be affected by esophageal inflammation or pressure caused by severe GERD. Although uncommon, significant reflux could theoretically contribute to irritation along the phrenic nerve’s course. Furthermore, individuals with GERD often experience anxiety or stress related to their symptoms, which are known triggers for muscle spasms, including those affecting the diaphragm. The cyclical nature of GERD – symptom flare-ups leading to anxiety, further exacerbating spasms – can create a frustrating and challenging situation.
It’s also important to consider that diaphragmatic spasms themselves aren’t necessarily indicative of GERD. They can occur independently due to various reasons such as dehydration, electrolyte imbalances (like low potassium or magnesium), stress, rapid eating, carbonated beverages, or even changes in temperature. Therefore, determining if a spasm is related to GERD requires careful evaluation and consideration of the broader clinical picture. It’s critical not to self-diagnose; instead, seek professional medical advice to pinpoint the underlying cause. Consider also understanding the liver’s role as it relates to overall health and digestion.
Identifying Diaphragmatic Spasms: Symptoms & Differentiation
Diaphragmatic spasms can manifest in a variety of ways, making diagnosis tricky. The most common symptom is a sudden tightening or cramping sensation in the chest or upper abdomen. This spasm typically lasts only a few seconds to minutes but can be quite intense and alarming. Unlike heartburn which often burns up from the stomach, diaphragmatic spasms are frequently described as a squeezing or constricting feeling. It’s important to differentiate these spasms from other conditions that present with similar symptoms like:
- Cardiac issues: Chest pain associated with heart problems is often more prolonged and may radiate to the arm, jaw, or back. It’s usually accompanied by shortness of breath, sweating, or dizziness.
- Musculoskeletal pain: Muscle strains or injuries in the chest wall can also cause localized pain but tend to be related to specific movements or activities.
- Panic attacks: Anxiety and panic disorders can mimic diaphragmatic spasms through hyperventilation and muscle tension.
Distinguishing between these conditions requires careful evaluation by a healthcare professional. Specific characteristics that may suggest diaphragmatic spasm include: the sudden onset and offset of the sensation, its tendency to occur sporadically, and lack of radiation or accompanying symptoms typical of heart problems. Often, the spasms are worse after eating or lying down—a pattern consistent with GERD exacerbation. It’s important to remember the connection between gerd and other related symptoms.
The Role of Esophageal Motility Disorders
Esophageal motility disorders – conditions affecting how the esophagus contracts to move food down to the stomach – can frequently coexist with GERD and contribute to diaphragmatic spasms. Achalasia, for example, is a rare disorder where the lower esophageal sphincter (LES) doesn’t relax properly, making it difficult for food to pass into the stomach. This leads to food accumulating in the esophagus, causing discomfort and potentially triggering spasms in both the esophageal muscles themselves and indirectly affecting the diaphragm.
Another motility issue, nutcracker esophagus, involves overly strong contractions of the esophageal muscles during swallowing. While not directly impacting the diaphragm, the intense pressure created by these contractions can sometimes be felt as chest discomfort or even radiate to the diaphragm area, mimicking a spasm. Furthermore, chronic GERD itself can disrupt normal esophageal motility over time. The constant exposure to acid irritates and damages the esophagus, altering its contractile function and potentially leading to dysmotility that exacerbates symptoms and increases the likelihood of spasms. This is also where understanding bile’s role can be beneficial in understanding digestion as a whole.
Managing Diaphragmatic Spasms Related to GERD
Managing diaphragmatic spasms linked to GERD requires a multi-faceted approach focused on both controlling the underlying reflux and addressing the spasm itself. The first step is effective GERD management, which typically involves:
- Lifestyle Modifications: These are often the cornerstone of treatment and include dietary changes (avoiding trigger foods like caffeine, alcohol, chocolate, fatty foods), elevating the head of your bed during sleep, losing weight if overweight, and quitting smoking.
- Medications: Over-the-counter antacids can provide temporary relief from heartburn, while proton pump inhibitors (PPIs) or H2 receptor antagonists may be prescribed by a doctor to reduce acid production. Understanding antacid’s role can help you make informed decisions about treatment options.
- Stress Management: Techniques like deep breathing exercises, yoga, meditation, and mindfulness can help reduce anxiety and tension that may contribute to spasms.
For the spasm itself, several strategies can offer relief:
- Diaphragmatic Breathing: Practicing slow, deep breaths focusing on expanding the diaphragm can sometimes calm muscle contractions.
- Gentle Stretching: Light stretching exercises targeting the chest and abdomen may help relieve tension.
- Hydration: Staying adequately hydrated helps maintain electrolyte balance, which is crucial for proper muscle function.
- Warm Compresses: Applying a warm compress to the chest or abdomen can soothe discomfort.
It’s also important to consider the role of chewing gum as an alternative management technique for GERD. Finally, remember food and mood’s link – a healthy diet can contribute to overall wellbeing and potentially reduce stress levels.
Important Disclaimer: This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. Self-treating can be dangerous, and proper diagnosis and management are crucial for both GERD and diaphragmatic spasms.