Chest pain is one of those symptoms that immediately triggers anxiety in many people, understandably so. The heart resides in the chest, making it easy to assume any discomfort there signals a potentially life-threatening cardiac event. However, chest pain is remarkably diverse in its origins, and often stems from issues completely unrelated to the cardiovascular system. Gastroesophageal Reflux Disease (GERD), a common digestive disorder, can frequently mimic cardiac pain, leading to confusion and unnecessary worry. Understanding the nuances between these two sources of discomfort – digestive versus cardiac – is crucial for appropriate assessment and care. This article will delve into the complexities of GERD-related chest pain, how it differs from heart-related pain, and what steps individuals can take when experiencing these symptoms.
The challenge lies in the overlap of symptoms. Both GERD and heart problems can cause discomfort described as tightness, pressure, burning, or aching in the chest. This similarity is why many people initially assume a cardiac issue when heartburn flares up. Furthermore, anxiety surrounding potential heart problems can exacerbate both GERD symptoms and the perception of pain, creating a vicious cycle. It’s important to remember that self-diagnosis is never recommended, and any new or worsening chest pain warrants medical evaluation, but understanding the characteristics of each source can empower individuals to communicate effectively with healthcare professionals and navigate their concerns more confidently. Understanding how stress and mental health affect digestive health is also key in this process.
Understanding GERD and Chest Pain
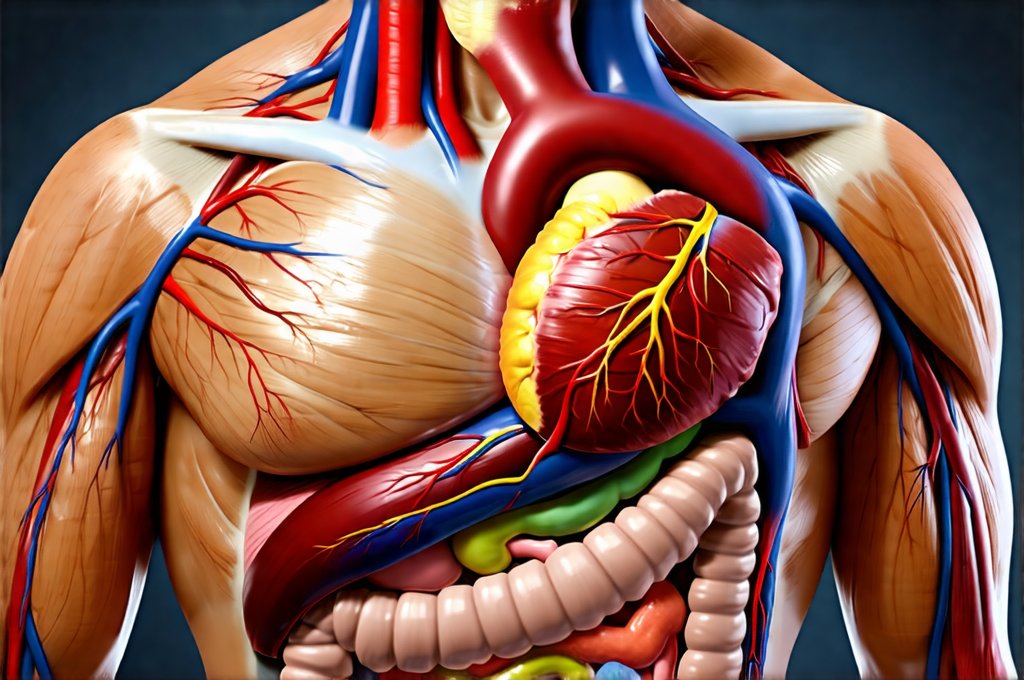
Gastroesophageal Reflux Disease (GERD) occurs when stomach acid frequently flows back into the esophagus – the tube connecting your mouth to your stomach. This backflow, known as acid reflux, irritates the lining of the esophagus, causing heartburn, regurgitation, and sometimes, chest pain. The lower esophageal sphincter (LES), a muscular valve at the bottom of the esophagus, is meant to prevent this backflow. When the LES weakens or relaxes inappropriately, acid can escape. Several factors contribute to GERD, including diet, lifestyle choices, obesity, pregnancy, and certain medications. It’s not simply about the amount of acid produced; it’s the ability of the LES to contain it that’s often the issue. Balancing digestive fluids and pancreatic output can also play a role in managing GERD symptoms.
The chest pain associated with GERD isn’t usually the sharp, crushing pain typically linked to heart attacks. Instead, it tends to be a burning sensation behind the breastbone, sometimes radiating toward the throat or back. This pain can be atypical, meaning it doesn’t fit the classic “textbook” description of either cardiac or digestive discomfort. It might also occur after eating, when lying down, or bending over – all positions that encourage acid reflux. Importantly, GERD-related chest pain often improves with antacids or other acid-reducing medications. This is a key differentiator from heart-related pain, which typically doesn’t respond to these treatments.
Many individuals experience silent reflux, where they have symptoms of GERD without the typical heartburn. This can still cause chest pain and even damage to the esophagus over time, making it harder to detect without medical investigation. The presence of other GERD symptoms like a sour taste in the mouth, chronic cough, or difficulty swallowing should raise suspicion even if heartburn isn’t present. Long-term, untreated GERD can lead to more serious complications such as esophagitis (inflammation of the esophagus), esophageal strictures (narrowing of the esophagus), and Barrett’s esophagus (a precancerous condition). Breaking the loop of anxiety and digestive chaos can prevent these complications.
Differentiating Cardiac Chest Pain from GERD
Cardiac chest pain, often referred to as angina, is usually caused by reduced blood flow to the heart muscle. This can occur due to coronary artery disease – a buildup of plaque in the arteries that supply the heart. The sensation is frequently described as a squeezing, pressure, tightness, or heavy weight on the chest. Unlike GERD-related pain, it’s less likely to be burning and isn’t typically relieved by antacids. Cardiac pain can radiate to the left arm, jaw, neck, back, or shoulder, and may be accompanied by shortness of breath, sweating, nausea, dizziness, or a feeling of impending doom. These are red flag symptoms that demand immediate medical attention.
A crucial difference lies in how the pain is triggered. While GERD chest pain often follows meals or specific positions, cardiac pain may occur during exertion (exercise-induced angina) or even at rest (unstable angina). The duration also differs. Cardiac pain can last for several minutes to hours, whereas GERD-related pain tends to be more intermittent and shorter in duration. It’s important to remember that heart attacks don’t always present with textbook symptoms. Some individuals experience atypical presentations, making diagnosis challenging. Finding the line between picky eating and digestive discomfort can help identify underlying conditions contributing to cardiac issues.
It is vital to understand that these are general guidelines; there’s considerable variability between individuals. A healthcare professional will consider your medical history, risk factors (such as age, family history of heart disease, smoking status), and perform a thorough examination to determine the cause of chest pain. Diagnostic tests like an electrocardiogram (ECG), blood tests, stress test, or echocardiogram may be necessary to rule out cardiac issues definitively. If digestive issues arise after surgery, review K91 — Digestive issues after surgery: What to expect and manage.
When to Seek Immediate Medical Attention
Regardless of whether you suspect GERD or a heart problem, certain symptoms always warrant immediate medical attention. These include:
- Severe chest pain that is crushing, squeezing, or feels like a heavy weight
- Chest pain accompanied by shortness of breath, sweating, nausea, vomiting, dizziness, or lightheadedness
- Pain radiating to the left arm, jaw, neck, or back
- Sudden onset of intense chest pain
- Feeling of impending doom
These symptoms could indicate a heart attack or other serious cardiac event and require prompt diagnosis and treatment. Don’t hesitate to call emergency services (911 in many countries) if you experience any of these warning signs – it’s always better to err on the side of caution. Waiting to see if the pain subsides can have life-threatening consequences.
Diagnostic Tools for Chest Pain Evaluation
When evaluating chest pain, healthcare professionals utilize a variety of diagnostic tools. An electrocardiogram (ECG) records the electrical activity of the heart and can help identify arrhythmias or signs of ischemia (reduced blood flow). Blood tests can measure cardiac enzymes – substances released into the bloodstream when heart muscle is damaged. A stress test assesses how well your heart functions during exercise, revealing potential blockages in coronary arteries. An echocardiogram uses ultrasound to create images of your heart, allowing doctors to evaluate its structure and function.
For suspected GERD, diagnostic tests may include:
- Endoscopy: A thin, flexible tube with a camera is inserted into the esophagus to visualize the lining and identify any inflammation or damage.
- Ambulatory reflux monitoring: This test measures the amount of acid in your esophagus over 24 hours, helping to diagnose GERD even if heartburn isn’t prominent.
- Esophageal manometry: Measures the pressure and function of the LES and esophageal muscles.
Managing GERD-Related Chest Pain & Prevention
If your chest pain is determined to be related to GERD, lifestyle modifications and medical treatments can help manage symptoms and prevent future episodes. Lifestyle changes include:
- Avoiding trigger foods (spicy foods, fatty foods, chocolate, caffeine, alcohol)
- Eating smaller, more frequent meals
- Elevating the head of your bed by 6-8 inches
- Losing weight if overweight or obese
- Quitting smoking
- Managing stress
Medical treatments may include:
- Antacids: Neutralize stomach acid for quick relief.
- H2 blockers: Reduce acid production.
- Proton pump inhibitors (PPIs): More potent acid suppressors, often used for long-term management of GERD.
- In some cases, surgery to strengthen the LES might be considered.
It’s important to work with your healthcare provider to determine the most appropriate treatment plan based on the severity of your symptoms and overall health. While GERD can cause significant discomfort, it’s often manageable with lifestyle changes and medical intervention, allowing individuals to live comfortable and productive lives. Remember that consistently monitoring for any changes in pain characteristics or new symptom development is crucial, ensuring timely evaluation if needed. Balancing digestive fluids and pancreatic output can also contribute to overall health management. And remember balancing structure and flexibility in digestive routines is key for a healthy lifestyle.