Gastroesophageal reflux disease (GERD) is frequently discussed in terms of heartburn and indigestion, but its reach extends far beyond these common symptoms. Many individuals experiencing chronic sinus issues – congestion, postnasal drip, recurring sinusitis – may not realize a connection exists between their digestive system and nasal passages. This seemingly odd pairing arises from the intricate physiological relationships within the body, specifically how stomach acid and mucus interact when reflux occurs. Understanding this interplay is crucial for accurately diagnosing the root cause of these symptoms and developing effective management strategies. It’s important to remember that while many experience occasional heartburn or sinus issues, persistent or severe symptoms warrant medical evaluation. You might also find helpful information regarding acid reflux and chest pain if you are concerned about these symptoms.
The link between GERD and sinus drainage isn’t as straightforward as it might seem. Acid reflux doesn’t directly cause a cold or sinusitis in the traditional sense of viral or bacterial infection. Instead, it creates an environment that can exacerbate existing sinus problems or even mimic them. When stomach acid backs up into the esophagus – and sometimes beyond – it can trigger inflammation and irritation not only in the esophageal lining but also higher up, affecting the sinuses and nasal passages. This happens through several mechanisms including vagal nerve stimulation, microaspiration of refluxed material into the airways, and immune responses to the acidic environment. The result is often an increase in mucus production, congestion, and a persistent feeling of fullness or blockage in the nose and throat. If you struggle with these issues, understanding when gas and bloating disrupt your day can also be beneficial.
Understanding the Connection: Acid’s Journey Upward
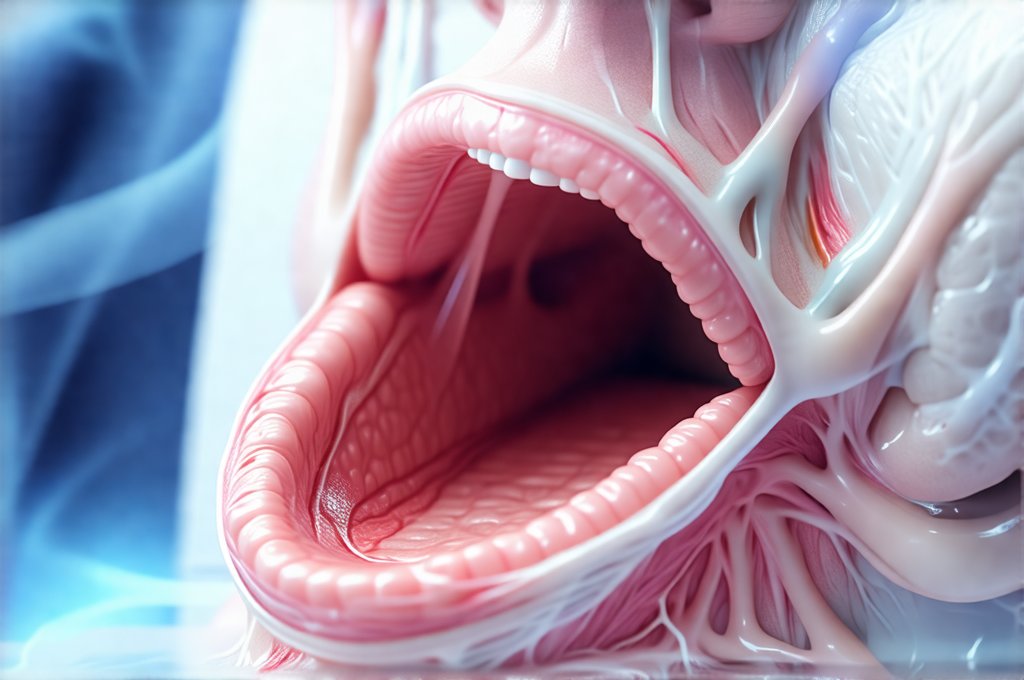
The lower esophageal sphincter (LES) is designed to prevent stomach acid from flowing back up into the esophagus. However, this valve can weaken or malfunction, allowing reflux to occur. Factors contributing to LES dysfunction include obesity, pregnancy, smoking, certain medications, and hiatal hernia. When acid escapes, it doesn’t just stay in the esophagus. It can travel further, reaching the throat and even the nasal passages during sleep when we are lying flat. This is known as laryngopharyngeal reflux (LPR), sometimes referred to as “silent reflux” because it often lacks typical heartburn symptoms. LPR is particularly relevant to sinus issues, as the proximity of the upper airway makes it susceptible to acid exposure.
- The acidic environment irritates the sensitive lining of the sinuses and nasal passages.
- This irritation stimulates mucus production as a protective mechanism, leading to congestion.
- Repeated or chronic exposure can lead to inflammation and even secondary infections.
The impact isn’t limited to direct acid contact either. Refluxed material contains enzymes like pepsin which further irritate the upper airway. Moreover, the body’s attempt to neutralize the acid can also contribute to symptoms. The increased mucus production, while initially protective, becomes problematic when it thickens and obstructs sinus drainage, creating a vicious cycle of congestion and discomfort. It’s vital to recognize that this isn’t always about severe, burning heartburn; often, the symptoms are subtle but persistent – a chronic stuffy nose, frequent clearing of the throat, or a sensation of something dripping down the back of the throat (postnasal drip). It is also worth investigating acid reflux and sinus issues to gain more insight.
Sinus Drainage & Reflux Symptoms: What Does it Look Like?
Differentiating between allergy-related sinus issues and reflux-related sinus problems can be tricky. Both conditions share overlapping symptoms. However, key distinctions can help guide diagnosis. Allergy symptoms typically fluctuate with pollen counts or exposure to allergens, are often accompanied by itchy eyes and sneezing, and respond well to antihistamines. Reflux-related sinus symptoms, conversely, may worsen after meals, when lying down, or at night. They might also be associated with other GERD symptoms like heartburn, regurgitation (though as mentioned before, these aren’t always present), or a sour taste in the mouth.
Here are some common signs that your sinus drainage could be linked to GERD:
– Chronic congestion without clear allergic triggers.
– Postnasal drip that feels thick and sometimes acidic tasting.
– Recurring sinusitis, even after antibiotic treatment.
– Worsening symptoms when lying down or after eating.
– A persistent cough, particularly at night.
It’s important to note the variability of these symptoms. Some individuals might experience severe congestion while others primarily struggle with postnasal drip. The presentation depends on individual physiology and the extent of reflux. Moreover, many people have both allergies and GERD, making diagnosis even more complex. This is where a thorough medical evaluation by an ENT (ear, nose, and throat) specialist or gastroenterologist is crucial. They can perform tests to assess esophageal function, identify acid exposure in the upper airway, and rule out other potential causes of your symptoms. Sometimes identifying why IBS and gas symptoms flare when you’re overwhelmed can help to understand a patient’s overall health picture.
Diagnosing the Link: Testing & Evaluation
Accurately diagnosing reflux-related sinus issues requires a multi-faceted approach. A simple physical exam might provide initial clues, but more specific testing is often needed to confirm the diagnosis and determine the severity of reflux. One common test is esophageal manometry, which measures the pressure within the esophagus and assesses LES function. This helps identify weaknesses or malfunctions in the valve that allow acid to escape. Another key test is 24-hour pH monitoring, where a small probe is placed in the esophagus to measure acid exposure over an extended period.
Beyond esophageal testing, your doctor might consider:
1. Laryngoscopy: A visual examination of the throat and larynx to look for signs of inflammation or irritation caused by refluxed acid.
2. Endoscopic Examination: Using a small camera to view the esophagus and stomach lining directly. This can help identify esophagitis (inflammation of the esophagus) or other abnormalities.
3. Allergy testing: Ruling out allergic rhinitis as a primary cause of sinus symptoms is essential, even if GERD is suspected.
It’s also important to maintain a detailed symptom diary, noting when your congestion and postnasal drip worsen – after meals, at night, during exercise – to help identify patterns and potential triggers. This information can be invaluable for your doctor in making an accurate diagnosis. Remember that the goal isn’t just to identify reflux but to understand how it’s impacting your sinuses specifically. If more serious problems are suspected, you may need a liver biopsy.
Lifestyle Modifications: Your First Line of Defense
For many individuals with mild to moderate reflux-related sinus issues, lifestyle modifications are often the first step in management. These changes aim to reduce acid production, prevent reflux, and improve sinus drainage. Dietary adjustments play a significant role – avoiding trigger foods like caffeine, alcohol, chocolate, spicy foods, fatty foods, and citrus fruits can help minimize acid production. Eating smaller, more frequent meals rather than large ones also reduces the risk of reflux.
Other helpful lifestyle modifications include:
– Elevating the head of your bed by 6-8 inches to prevent nighttime reflux.
– Avoiding eating within 2-3 hours of bedtime.
– Maintaining a healthy weight. Obesity increases intra-abdominal pressure, contributing to reflux.
– Quitting smoking. Smoking weakens the LES and irritates the esophageal lining.
Furthermore, proper hydration is crucial for thinning mucus and promoting sinus drainage. Using a saline nasal rinse or neti pot can also help clear congestion and remove irritants from the nasal passages. These measures often provide significant relief for mild cases of reflux-related sinus issues. However, if symptoms persist despite lifestyle changes, medical intervention may be necessary.
Medical Management: Beyond Lifestyle Changes
When lifestyle modifications are insufficient, several medical treatments can help manage GERD and alleviate associated sinus problems. Proton pump inhibitors (PPIs) are commonly prescribed to reduce stomach acid production. These medications are highly effective but should be used under the guidance of a doctor, as long-term use can have potential side effects. Other medications include H2 receptor antagonists, which also reduce acid production, and prokinetic agents, which help speed up gastric emptying and strengthen the LES.
In some cases, surgery may be considered to reinforce the LES or address hiatal hernia. However, this is typically reserved for severe cases that don’t respond to other treatments. It’s vital to work closely with your healthcare team – including a gastroenterologist and ENT specialist – to develop a personalized treatment plan tailored to your specific needs and symptoms. The goal isn’t just symptom relief but also preventing long-term complications and improving overall quality of life. Remember, consistent monitoring and adjustments to the treatment plan may be necessary over time. If you are concerned about potential liver issues, recognizing the signs of liver failure is essential.