Gastroesophageal reflux disease (GERD), commonly known as acid reflux, affects millions worldwide, presenting primarily with heartburn and regurgitation. However, many individuals experience symptoms beyond these typical digestive complaints – often reporting pain in the upper back and chest that can be easily mistaken for musculoskeletal issues. This leads to a complex diagnostic challenge because the interplay between gastrointestinal health and spinal discomfort isn’t always immediately apparent. Understanding this potential connection is crucial for accurate diagnosis and effective treatment, preventing years of misdirected therapy focused solely on the spine while the underlying digestive issue remains unaddressed.
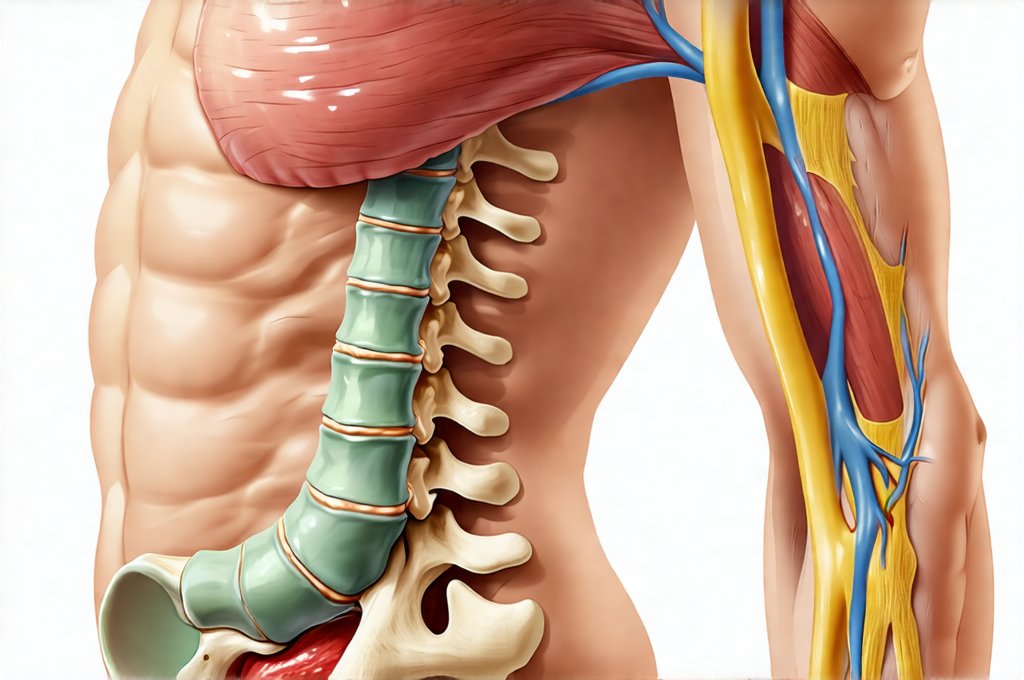
The relationship between GERD and upper back pain isn’t a simple cause-and-effect scenario; it’s more accurately described as a complex interaction involving referred pain, muscle tension, and potentially altered biomechanics resulting from chronic discomfort. The esophagus, the muscular tube connecting your mouth to your stomach, sits relatively close to the thoracic spine—the region of the back between the neck and lower back. When acid reflux occurs repeatedly, it can cause inflammation and irritation not only in the esophagus but also in surrounding tissues, including those impacting spinal nerves and muscles. This creates a pathway for pain signals to be misinterpreted or felt in areas seemingly unrelated to the digestive system. Moreover, chronic discomfort from GERD frequently leads to postural changes and muscle guarding, further exacerbating back pain.
Understanding the Digestive-Spinal Link
The mechanism behind referred pain is vital to understanding how GERD can manifest as upper back pain. Referred pain occurs when a painful stimulus in one part of the body is perceived as originating from another location. This happens because nerve fibers share pathways and the brain sometimes struggles to pinpoint the exact source of discomfort. In the case of GERD, irritation of the esophagus or even spasms within the esophageal muscles can send signals that are interpreted by the brain as coming from the upper back. The vagus nerve, a major cranial nerve heavily involved in digestion, also plays a role; its pathways connect the digestive system to various regions of the body, including the spine, potentially contributing to this phenomenon.
Beyond referred pain, the inflammatory response triggered by GERD can contribute significantly to muscle tension and discomfort. Chronic acid exposure irritates the esophagus, prompting the body’s natural healing mechanisms to kick in. However, prolonged inflammation can lead to muscle spasms in the back and shoulder girdle as the body attempts to protect itself from further irritation or perceived threat. This creates a vicious cycle: GERD causes inflammation, leading to muscle tension, which then exacerbates discomfort and potentially worsens reflux symptoms due to altered abdominal pressure or posture.
Finally, it’s important to acknowledge that individuals experiencing chronic GERD often modify their posture unconsciously in an attempt to alleviate their symptoms. Leaning forward, hunching the shoulders, or adopting other awkward positions can all put undue stress on the spinal muscles and joints, leading to mechanical back pain independent of, yet intertwined with, the digestive issue. This makes distinguishing between purely musculoskeletal pain and GERD-related back pain particularly challenging. Considering [gut pain] and its triggers is key for diagnosis.
Diagnosing the Connection & Differentiating Pain Sources
Accurately diagnosing the source of upper back pain requires a comprehensive approach that considers both gastrointestinal and musculoskeletal factors. A thorough medical history is paramount; clinicians should specifically inquire about digestive symptoms alongside details about the location, intensity, and nature of the back pain. Questions regarding heartburn, regurgitation, difficulty swallowing (dysphagia), bloating, and any dietary triggers can provide valuable clues. Physical examination focusing on spinal range of motion, muscle tenderness, and neurological function is also essential to rule out purely mechanical causes of back pain such as strained muscles or herniated discs.
However, relying solely on these methods isn’t always sufficient. Endoscopy, a procedure where a thin, flexible tube with a camera is inserted into the esophagus, allows for direct visualization of esophageal inflammation and potential damage caused by acid reflux. Esophageal manometry, which measures the pressure within the esophagus during swallowing, can help identify motility disorders that may contribute to GERD symptoms. Furthermore, pH monitoring – either through ambulatory methods (a probe placed in the esophagus for 24-48 hours) or impedance testing—can quantify the amount of acid exposure over time and confirm the diagnosis of GERD. It’s critical to differentiate between pain originating from the spine versus being referred from the digestive system, requiring a careful assessment by healthcare professionals. If symptoms are worse [in the morning], further investigation is warranted.
It’s also important to consider “red flag” symptoms that warrant further investigation beyond GERD. These include severe or worsening back pain accompanied by neurological deficits (weakness, numbness, tingling), fever, unexplained weight loss, or bowel/bladder dysfunction—which could indicate more serious underlying conditions unrelated to digestion. In these cases, imaging studies like X-rays, CT scans, or MRIs of the spine may be necessary to rule out other causes of back pain.
The Role of Lifestyle Modifications
Lifestyle modifications form the cornerstone of GERD management and can often significantly reduce both digestive symptoms and associated back pain. These include: – Elevating the head of your bed by 6-8 inches to help prevent nighttime reflux. – Avoiding trigger foods such as caffeine, alcohol, chocolate, fatty foods, and spicy foods. – Eating smaller, more frequent meals instead of large ones. – Losing weight if overweight or obese, as excess abdominal pressure can contribute to GERD. – Quitting smoking, as nicotine weakens the lower esophageal sphincter (LES). – Avoiding lying down immediately after eating.
Dietary adjustments are particularly important; identifying and eliminating personal trigger foods can dramatically reduce acid production and reflux episodes. Maintaining a food diary for several weeks can help pinpoint problematic items. Furthermore, mindful eating practices – such as chewing thoroughly and slowing down meal pace—can improve digestion and minimize symptoms. These changes not only address the root cause of GERD but also indirectly alleviate back pain by reducing inflammation and muscle tension. Understanding [the liver’s role] in detoxification is also beneficial.
Medications & Their Impact on Spinal Comfort
When lifestyle modifications aren’t sufficient to control GERD symptoms, medications may be necessary. Proton pump inhibitors (PPIs) are commonly prescribed to reduce acid production in the stomach, while H2 receptor antagonists offer a milder form of acid suppression. Antacids provide quick relief from heartburn but don’t address the underlying cause. The effectiveness of these medications in reducing back pain is often indirect; by controlling GERD symptoms, they minimize inflammation and muscle tension that contribute to spinal discomfort.
However, it’s important to note that some medications can have side effects that potentially worsen musculoskeletal issues. For example, long-term PPI use has been linked to decreased magnesium absorption, which can lead to muscle cramps and spasms. Therefore, healthcare providers should carefully assess the benefits and risks of medication therapy and consider alternative approaches whenever possible. Additionally, physical therapy focusing on strengthening core muscles and improving posture can complement medical treatment and provide lasting relief from back pain. [Balancing structure] in routines is crucial for consistent management.
The Importance of a Multidisciplinary Approach
Managing GERD-related upper back pain often requires a collaborative approach involving multiple healthcare professionals. A gastroenterologist can diagnose and treat the underlying digestive issue, while a physical therapist can address musculoskeletal imbalances and provide targeted exercises to improve posture and strengthen supporting muscles. Pain management specialists may be involved in cases of chronic or severe pain.
Effective communication between these practitioners is crucial to ensure coordinated care and prevent misdiagnosis or conflicting treatments. Patients should actively participate in their own care by providing detailed information about their symptoms, responding honestly to questions, and adhering to recommended treatment plans. A holistic approach that integrates both digestive health and spinal well-being offers the best chance of achieving long-term relief and improving quality of life for individuals experiencing this complex interplay between GERD and upper back pain. It’s vital to remember that what feels like a purely back problem may have its origins in digestive health, and recognizing that connection is the first step towards effective treatment. Those struggling with discomfort should consider [emotional triggers] as well. And it’s important to understand how [seafood and digestive discomfort] can play a role. Finally, if you suspect issues are related to [picky eating], seek professional guidance.