Gastroesophageal reflux disease (GERD) is a surprisingly common condition, affecting millions worldwide. Often dismissed as merely “heartburn,” GERD’s impact extends far beyond that burning sensation in the chest. While many associate it with digestive symptoms like acid regurgitation and bloating, a less recognized but significant manifestation of GERD can be pain and discomfort in the upper back – often linked to heightened nerve sensitivity. This connection isn’t always immediately obvious, leading to misdiagnosis or delayed treatment, leaving individuals frustrated and searching for answers. Understanding this interplay between digestive health and neurological responses is crucial for effective management and improved quality of life.
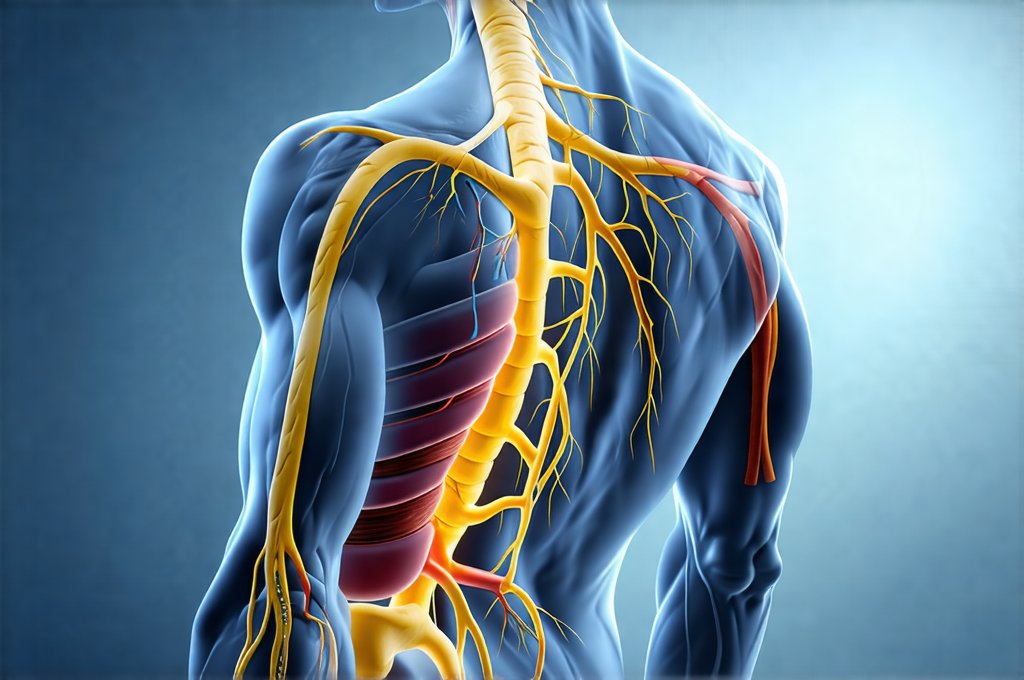
The complexity arises because GERD doesn’t just irritate the esophagus; it can trigger a cascade of physiological reactions that impact the nervous system. Chronic inflammation from reflux can sensitize nerves, leading to heightened pain perception in areas seemingly distant from the stomach. This phenomenon, known as visceral hypersensitivity, means individuals may experience more intense and prolonged pain even with relatively minor stimulation. Furthermore, the vagus nerve—a crucial communication pathway between the gut and the brain—plays a significant role, potentially exacerbating these sensations. Recognizing this intricate connection is vital for holistic care that addresses not only the digestive symptoms but also the associated neurological effects. You can learn more about the role of the vagus nerve in similar conditions.
The Gut-Brain Axis and GERD
The relationship between our digestive system and our brain isn’t one-way; it’s a dynamic two-way communication network called the gut-brain axis. This axis involves complex interactions via neural, hormonal, and immunological pathways. In essence, what happens in your gut profoundly influences your brain, and vice versa. GERD disrupts this delicate balance. Chronic acid reflux causes inflammation which then sends signals to the brain, potentially altering pain processing and increasing sensitivity.
- Inflammation can directly stimulate nerve endings in the esophagus and stomach.
- These nerves transmit signals to the brain via the vagus nerve.
- The brain interprets these signals as pain or discomfort.
- Prolonged stimulation leads to sensitization, meaning less stimulus is required to trigger a painful response.
This sensitization isn’t limited to the digestive tract; it can spread to other areas, including the upper back. The thoracic spine and surrounding musculature often become focal points for this referred pain due to shared nerve pathways and anatomical proximity. The brain may misinterpret signals originating from the esophagus as coming from the back, leading to localized pain even without any structural issues in the spine itself. It’s important to note that this isn’t “imaginary” pain; it’s a genuine neurological response to physiological changes caused by GERD. Understanding the difference between allergy and sensitivity can also provide context for inflammatory responses in the body.
The vagus nerve is particularly critical here. It’s responsible for regulating numerous bodily functions, including digestion and heart rate. In GERD, chronic irritation can affect the vagus nerve’s function, leading to altered signaling and increased sensitivity to pain signals. This creates a vicious cycle: reflux irritates the esophagus, sensitizes the vagus nerve, and amplifies pain perception, potentially contributing to upper back discomfort. Addressing this axis is therefore essential for comprehensive management of GERD symptoms beyond simple acid suppression. The impact of gut microbiome in food sensitivity can also play a role here, influencing nerve function.
Understanding Visceral Hypersensitivity
Visceral hypersensitivity is a key factor in understanding why some individuals with GERD experience significant upper back pain while others don’t. It refers to an increased sensitivity to stimuli within the internal organs (viscera). Normally, our bodies can tolerate a certain amount of distension or irritation in the gut without registering it as painful. However, in visceral hypersensitivity, even mild stimulation triggers a disproportionately strong pain response.
This isn’t simply about having a “low pain threshold.” It’s a neurological phenomenon involving changes in how the brain processes signals from the viscera. Chronic inflammation associated with GERD can alter nerve function and reduce the inhibitory mechanisms that normally dampen down pain signals. As a result, the brain becomes hyper-vigilant to gut sensations, perceiving even normal digestive activity as painful. This heightened sensitivity isn’t limited to the esophagus; it can extend to other areas of the body, including the upper back, leading to referred pain and chronic discomfort. Understanding the role of bile in digestion is also important as it contributes to overall digestive function.
Managing visceral hypersensitivity requires a multifaceted approach beyond simply reducing stomach acid. Strategies like stress management techniques (yoga, meditation), dietary modifications, and potentially neuromodulation therapies (under medical guidance) can help recalibrate pain processing and reduce sensitivity over time. It’s crucial to remember that this is a neurological issue, not just a digestive one, requiring a broader perspective on treatment.
The Role of Nerve Entrapment & Musculoskeletal Factors
While GERD-related nerve sensitization is often the primary driver of upper back pain, it’s vital to rule out other potential causes. Nerve entrapment—where nerves are compressed or irritated by surrounding tissues—can mimic GERD-related pain and may coexist with the condition. Musculoskeletal issues, such as muscle strains or spinal dysfunction, can also contribute to discomfort in the upper back.
It’s important to distinguish between pain directly caused by GERD’s impact on nerve sensitivity and pain originating from structural problems in the spine or surrounding muscles. A thorough physical examination by a healthcare professional is essential to identify any musculoskeletal issues that may be contributing to the symptoms. Often, these issues aren’t the root cause but can exacerbate the pain experience when combined with heightened nerve sensitivity from GERD.
- Physical therapy focusing on postural correction and muscle strengthening can help alleviate musculoskeletal contributions.
- Addressing underlying nerve entrapment (if present) through appropriate treatment modalities may be necessary.
- A comprehensive assessment is crucial to determine whether the pain is primarily GERD-related, musculoskeletal, or a combination of both.
Diagnostic Challenges & Seeking Appropriate Care
Diagnosing the link between GERD and upper back pain can be challenging because the symptoms are often non-specific. Many other conditions can cause similar pain, leading to misdiagnosis or delayed treatment. Doctors may initially focus on ruling out spinal problems before considering a digestive origin.
A detailed medical history, including questions about heartburn, acid regurgitation, bloating, and any relationship between meals and back pain, is crucial. Diagnostic tests for GERD, such as endoscopy, pH monitoring, and impedance testing, can help confirm the presence of reflux. However, these tests don’t directly assess nerve sensitivity or visceral hypersensitivity.
- Consider seeking a second opinion if your initial diagnosis doesn’t address your concerns.
- Look for healthcare professionals with experience in both gastroenterology and pain management.
- Be prepared to describe your symptoms in detail, including what makes them better or worse.
Effective treatment often requires a multidisciplinary approach involving gastroenterologists, neurologists, physical therapists, and potentially psychologists specializing in chronic pain management. Treatment may involve lifestyle modifications (dietary changes, weight loss), medications to reduce stomach acid, therapies to manage stress and anxiety, and rehabilitation programs to address musculoskeletal imbalances. Remember that self-treating is not advisable; always consult with qualified healthcare professionals for diagnosis and treatment.
Lifestyle and Management Strategies
Beyond medical interventions, several lifestyle modifications can significantly impact both GERD symptoms and nerve sensitivity. Dietary adjustments are paramount. Identifying and avoiding trigger foods – such as caffeine, alcohol, chocolate, spicy foods, and fatty meals – can reduce reflux episodes and minimize esophageal irritation. Eating smaller, more frequent meals rather than large ones also helps prevent overfilling the stomach and reducing pressure on the lower esophageal sphincter.
Regular exercise promotes overall health and well-being, but it’s essential to choose activities that don’t exacerbate GERD symptoms. Low-impact exercises like walking, swimming, or yoga are generally preferred over high-intensity activities that increase abdominal pressure. Maintaining a healthy weight is also crucial, as excess weight can contribute to reflux.
Stress management techniques are incredibly important given the gut-brain connection. Chronic stress can worsen GERD symptoms and heighten nerve sensitivity. Practices like meditation, deep breathing exercises, mindfulness, and progressive muscle relaxation can help reduce stress levels and improve overall coping mechanisms. Prioritizing sleep is also essential, as inadequate sleep can exacerbate both digestive issues and pain perception.
Finally, paying attention to posture can make a difference. Poor posture can compress the abdomen and increase pressure on the esophagus, potentially worsening reflux. Maintaining good posture while sitting and standing can help alleviate these pressures. These lifestyle changes are not quick fixes but rather ongoing strategies that contribute to long-term management of GERD and its associated nerve sensitivity. Remember to consult your healthcare provider before making significant dietary or exercise changes. Understanding the liver’s role in detox can also help you make informed lifestyle choices. It’s important to note that the connection between food and mood, especially in kids, can impact overall well-being and stress levels. Finally, consider exploring whether an enzyme deficiency may play a role in your digestive discomfort.