Gastroesophageal reflux disease (GERD), often manifesting as frequent heartburn or acid indigestion, is a surprisingly pervasive condition affecting millions worldwide. While commonly understood as a digestive issue, its impact extends far beyond the esophagus, increasingly recognized for influencing mental well-being and even seemingly unrelated aspects of daily life such as energy levels and motivation. Many individuals experiencing chronic GERD report feeling a persistent sense of fatigue, difficulty concentrating, and a general lack of drive – symptoms that often go unacknowledged as being connected to their digestive health. This creates a challenging cycle where the physical discomfort of GERD can contribute to mental and emotional distress, further exacerbating feelings of helplessness and hindering everyday functioning.
The connection isn’t simply anecdotal; growing research highlights a complex bidirectional relationship between the gut and the brain – often referred to as the gut-brain axis. This intricate communication network involves neurological pathways, hormonal signals, and immune responses that constantly relay information back and forth. Disruptions within the digestive system, like those caused by chronic GERD, can significantly influence brain function, impacting mood, motivation, and cognitive abilities. Understanding this link is crucial for developing holistic approaches to managing GERD that address not only the physical symptoms but also the associated mental and emotional challenges. It’s about recognizing that feeling “off” isn’t necessarily a sign of weakness or lack of willpower, but potentially a signal from your gut impacting your brain.
The Gut-Brain Axis and GERD
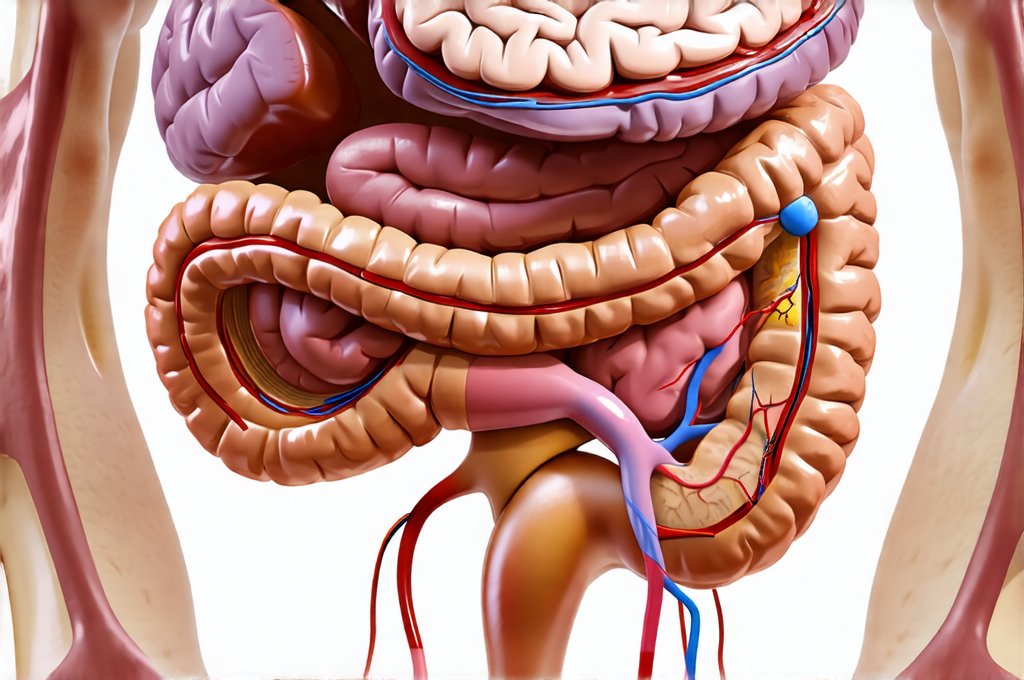
The gut-brain axis is far more than just a theoretical concept; it’s the physiological basis for the strong connection between digestive health and mental state. This two-way communication highway involves several key components:
– The vagus nerve, which directly connects the gut to the brain.
– Production of neurotransmitters in the gut – surprisingly, many “feel good” chemicals like serotonin are largely produced there.
– The microbiome—the trillions of bacteria residing in our intestines—which influence both physical and mental health.
– Immune system interactions; a significant portion of our immune system resides in the gut.
GERD’s chronic inflammation can disrupt this delicate ecosystem. Persistent acid reflux irritates the esophagus and, over time, contributes to systemic inflammation throughout the body. This inflammatory response isn’t confined to the digestive tract – it can reach the brain, impacting neurotransmitter production and potentially contributing to mood disorders and reduced motivation. Consider that chronic pain, a frequent companion of GERD, is known to deplete mental resources and decrease dopamine levels, directly affecting reward pathways and leading to feelings of apathy. The constant discomfort also triggers stress responses, further depleting energy reserves and hindering cognitive function. Furthermore, if you are experiencing persistent digestive issues, it may be time to consider recognizing symptoms of other conditions as well.
Furthermore, GERD symptoms often disrupt sleep. Poor sleep quality significantly impacts motivation – it reduces the brain’s ability to consolidate memories, impairs decision-making, and lowers overall energy levels. This creates a vicious cycle: GERD interferes with sleep, poor sleep diminishes motivation, and low motivation makes it harder to manage stress which then worsens GERD symptoms. Breaking this cycle requires acknowledging the interconnectedness of these factors and adopting strategies that address both physical and mental well-being. It’s not simply about suppressing acid; it’s about restoring balance within the gut-brain axis. Understanding zinc and magnesium roles can help support overall wellness as well.
Nutritional and Lifestyle Considerations
A cornerstone of managing GERD and its impact on motivation lies in dietary and lifestyle adjustments. While there isn’t a one-size-fits-all approach, several strategies consistently demonstrate positive results. Dietary modifications often focus on identifying and eliminating trigger foods – these vary widely between individuals but commonly include caffeine, alcohol, spicy foods, fatty meals, chocolate, and carbonated beverages. A food diary can be immensely helpful in pinpointing specific culprits. Beyond elimination, prioritizing a diet rich in anti-inflammatory foods is crucial.
– Fruits and vegetables (especially leafy greens).
– Lean proteins.
– Healthy fats (like omega-3 fatty acids from fish or flaxseeds).
– Fiber-rich foods.
Lifestyle changes are equally important. Maintaining a healthy weight reduces pressure on the stomach, minimizing reflux episodes. Regular exercise promotes digestion and stress reduction. Stress management techniques – such as yoga, meditation, or deep breathing exercises – can help mitigate the impact of chronic stress on both gut health and mental well-being. Avoiding eating large meals before bed is also vital, allowing sufficient time for digestion. Elevating the head of your bed during sleep can further reduce nighttime reflux. These aren’t quick fixes, but consistent implementation of these habits builds a foundation for improved digestive function and enhanced mental clarity. Open communication with loved ones may also help you navigate the challenges of chronic illness.
Addressing Low Motivation: A Multifaceted Approach
Low motivation stemming from chronic GERD isn’t simply laziness; it’s often a symptom of depleted energy reserves, disrupted neurotransmitter balance, and ongoing discomfort. Treating this requires a multifaceted approach that goes beyond medication. One effective strategy is behavioral activation, which involves intentionally scheduling activities – even small ones – to combat feelings of apathy. This doesn’t require feeling motivated beforehand; the act of engaging in activity can actually generate motivation over time. Start with incredibly manageable tasks, like taking a short walk or listening to music, and gradually increase complexity as energy levels allow.
Another key component is mindfulness. Practicing mindfulness helps you become more aware of your body’s signals, including GERD symptoms and their impact on your mood. This awareness allows you to respond to discomfort with compassion rather than frustration, reducing the stress cycle. Mindfulness techniques can also help identify negative thought patterns that contribute to feelings of helplessness and self-doubt. Consider incorporating short mindfulness exercises into your daily routine, even just a few minutes each day, to cultivate greater self-awareness and emotional regulation.
Finally, seeking professional support is invaluable. A therapist or counselor specializing in chronic illness can provide guidance on coping strategies, stress management techniques, and behavioral changes tailored to your specific needs. A registered dietitian can help you develop a personalized meal plan that minimizes GERD triggers while ensuring adequate nutritional intake. Remember that asking for help isn’t a sign of weakness; it’s a proactive step towards reclaiming your well-being and restoring your motivation. It’s about acknowledging that chronic illness impacts all facets of life, and seeking support is essential for navigating those challenges effectively. Recognizing liver enlargement symptoms can also provide peace of mind.
The Role of the Microbiome in Motivation
The gut microbiome plays a surprisingly significant role in influencing mood and motivation. A dysbiotic microbiome – an imbalance of bacteria – has been linked to increased inflammation, impaired neurotransmitter production, and altered brain function. GERD medications, particularly proton pump inhibitors (PPIs), can sometimes disrupt the microbiome, potentially exacerbating these issues. While PPIs are often necessary for managing GERD symptoms, it’s important to discuss potential strategies for mitigating their impact on gut health with your doctor.
Probiotic supplementation – introducing beneficial bacteria into the gut – is one avenue for restoring microbial balance. However, probiotic strains vary significantly in their effectiveness, and not all probiotics are created equal. It’s best to consult with a healthcare professional or registered dietitian to determine which strains might be most appropriate for your individual needs. Dietary interventions can also support microbiome health:
1. Consuming prebiotic-rich foods (like garlic, onions, bananas, and asparagus) feeds beneficial bacteria.
2. Limiting sugar and processed foods reduces the growth of harmful bacteria.
3. Incorporating fermented foods (like yogurt, kefir, sauerkraut, and kimchi) introduces diverse bacterial strains.
The emerging field of psychobiotics – probiotics specifically designed to impact mental health – holds promise for addressing the gut-brain connection in GERD sufferers. While research is still ongoing, studies suggest that certain probiotic strains can reduce anxiety, improve mood, and enhance cognitive function. The key takeaway is that nurturing your microbiome isn’t just about digestive health; it’s about supporting a healthy brain and fostering greater motivation. Emotional burnout can also significantly impact gut health, creating a vicious cycle.
Long-Term Management and Prevention
Managing GERD and its impact on motivation isn’t a passive process; it requires ongoing commitment to lifestyle adjustments and proactive self-care. Regular monitoring of symptoms, identifying triggers, and adapting strategies as needed are crucial for long-term success. Don’t fall into the trap of thinking that once symptoms subside, you can revert to old habits – consistency is key.
Preventing future flare-ups involves prioritizing stress management, maintaining a healthy weight, and adhering to a gut-friendly diet. Consider incorporating regular physical activity into your routine, not just for its physical benefits but also for its mood-boosting effects. Building a strong support network – connecting with friends, family, or support groups – can provide encouragement and accountability during challenging times.
Finally, remember that self-compassion is essential. Chronic illness often brings setbacks, and it’s important to treat yourself with kindness and understanding when symptoms flare up. Don’t blame yourself for experiencing low motivation; recognize it as a natural response to chronic discomfort. Focus on small victories, celebrate progress, and prioritize your well-being above all else. The journey towards managing GERD and reclaiming your motivation is a marathon, not a sprint – and with consistent effort and self-care, you can navigate the challenges and live a fulfilling life. If you are experiencing severe symptoms, it’s important to recognize liver failure signs and seek immediate medical attention.