Gastroesophageal reflux disease (GERD) is an incredibly common condition, affecting millions worldwide. Many people experience occasional heartburn, but GERD signifies a more persistent issue where stomach acid frequently flows back into the esophagus, causing irritation and potential damage. Beyond the typical symptoms like burning sensation in the chest and regurgitation, there’s often speculation about less obvious connections – specifically, how GERD might relate to blood pressure fluctuations. It’s not uncommon for individuals managing chronic conditions to wonder if seemingly unrelated symptoms are somehow intertwined, leading to anxiety and a search for answers. This article delves into the complex relationship between GERD and fluctuating blood pressure, separating common misconceptions from potential physiological links and exploring what current research suggests about this often-overlooked interaction.
The concern arises because both GERD and fluctuations in blood pressure – encompassing both hypertension (high blood pressure) and hypotension (low blood pressure) – are prevalent conditions with overlapping risk factors and potentially shared underlying mechanisms. Symptoms like dizziness, lightheadedness, or even feeling unwell after meals can be attributed to either condition, creating confusion for patients and sometimes leading to misdiagnosis. Furthermore, some medications used to manage GERD can have effects on cardiovascular function, adding another layer of complexity. Understanding whether there’s a genuine link, and if so, how these two conditions might influence each other is crucial for holistic patient care and effective management strategies. This isn’t about finding definitive cures but rather clarifying the current understanding based on available evidence.
The Physiological Connections: How GERD Might Impact Blood Pressure
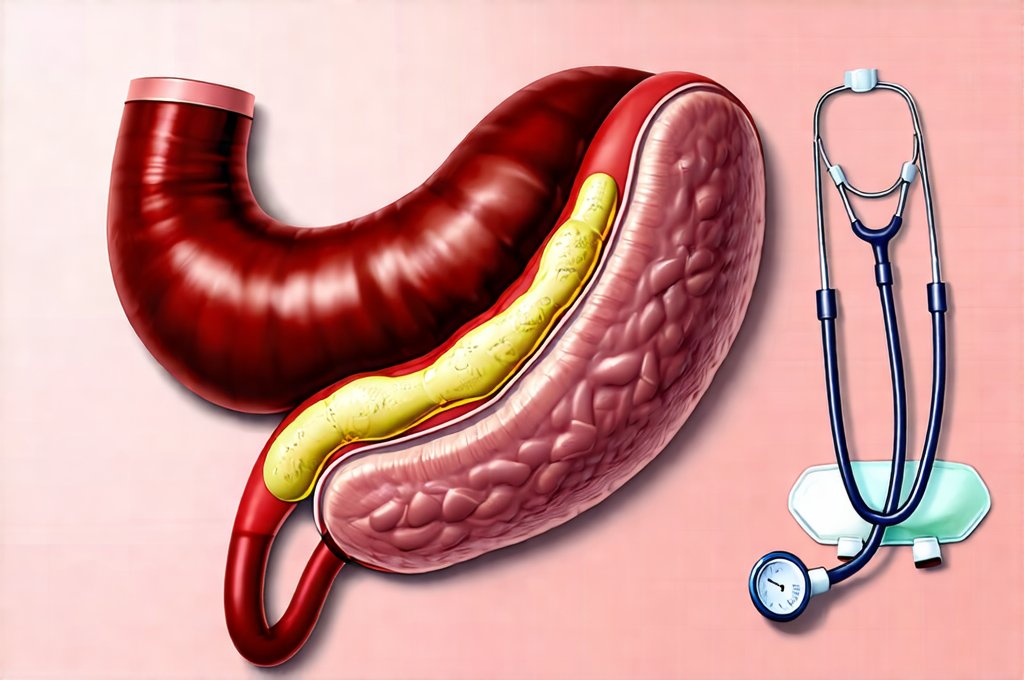
The relationship between GERD and blood pressure isn’t straightforward, but several physiological pathways could explain a potential connection. It begins with recognizing that the digestive system is intricately connected to the cardiovascular system. Vagal nerve stimulation plays a significant role here; this nerve connects the gut to the brain and heart, influencing both digestion and heart rate/blood pressure regulation. GERD, through inflammation and irritation of the esophagus, can stimulate the vagus nerve, potentially leading to changes in heart rhythm and blood pressure. This is particularly relevant because the act of swallowing itself triggers a vagal response.
Another key factor lies in the autonomic nervous system’s role in regulating both digestion and cardiovascular function. GERD-related discomfort or pain can trigger stress responses, activating the sympathetic nervous system – the “fight or flight” system – which raises blood pressure. Conversely, chronic inflammation associated with GERD can contribute to endothelial dysfunction, a condition where the inner lining of blood vessels doesn’t function optimally, potentially leading to hypertension over time. It’s not a direct cause-and-effect relationship but rather a complex interplay between inflammatory processes and nervous system regulation.
Finally, certain medications commonly used for GERD management might indirectly affect blood pressure. For instance, some antacids can influence electrolyte balance (like calcium levels), which has implications for cardiovascular function. Proton pump inhibitors (PPIs) – powerful acid-reducing drugs – have been the subject of research regarding potential cardiovascular side effects, though the evidence remains somewhat controversial and often depends on individual patient factors and duration of use. It’s important to note that discontinuing prescribed medication without a doctor’s guidance is never advisable. Understanding link between pancreatic health can also offer insight into overall systemic health.
GERD Medications & Blood Pressure: A Closer Look
The concern surrounding PPIs and blood pressure stems from several studies suggesting potential associations, but it’s essential to understand the nuances. Early research hinted at a possible link between long-term PPI use and an increased risk of cardiovascular events, including hypertension. The proposed mechanisms involved reduced nitric oxide production (nitric oxide helps relax blood vessels) due to altered stomach acid levels impacting absorption or metabolism of L-arginine – an amino acid essential for nitric oxide synthesis. However, subsequent larger studies have yielded mixed results, with some showing no significant association between PPIs and cardiovascular risk.
The current consensus leans towards caution rather than alarm. It’s crucial to remember that correlation doesn’t equal causation. Individuals taking PPIs often have other underlying health conditions or lifestyle factors (such as obesity, diabetes, or smoking) that contribute to cardiovascular disease independently of the medication. Moreover, the type and duration of PPI use may play a role; some PPIs might be more likely to interact with cardiovascular function than others. Doctors generally recommend using the lowest effective dose for the shortest necessary period to minimize potential risks. If you experience difficulties swallowing alongside GERD symptoms, consider exploring GERD and swallowing difficulties.
Regular blood pressure monitoring is vital for anyone on long-term GERD medication, particularly PPIs. If you experience changes in your blood pressure while taking these medications, it’s essential to discuss this with your healthcare provider. They can assess whether the medication might be contributing to the fluctuations and adjust your treatment plan accordingly – potentially exploring alternative strategies or monitoring for other cardiovascular risk factors. Managing GERD with esophagitis is essential to avoid complications.
The Role of Inflammation & Endothelial Function
Chronic inflammation is a hallmark of GERD. Repeated exposure to stomach acid irritates the esophageal lining, triggering an inflammatory response that extends beyond the esophagus itself. This systemic inflammation can contribute to endothelial dysfunction, damaging the inner walls of blood vessels and impairing their ability to dilate properly. Impaired dilation leads to increased vascular resistance and consequently elevates blood pressure. It’s a vicious cycle – GERD causes inflammation which damages blood vessels, potentially leading to hypertension, which then further exacerbates stress on the cardiovascular system.
Furthermore, chronic inflammation can also impact the autonomic nervous system, disrupting its ability to regulate blood pressure effectively. The sympathetic nervous system may become overactive, contributing to sustained elevations in blood pressure even when not triggered by acute stressors. This is why managing GERD symptoms and reducing inflammation are crucial components of overall cardiovascular health. Lifestyle modifications like dietary changes (reducing acidic foods, caffeine, alcohol), weight management, and stress reduction techniques can all help minimize inflammation and support healthy endothelial function. Sometimes bad breath is a symptom of GERD that requires attention.
Dietary Considerations & Vagal Tone Modulation
Diet plays a pivotal role in both GERD symptom management and blood pressure regulation. A diet rich in processed foods, saturated fats, and sodium contributes to inflammation and elevates blood pressure. Conversely, a diet abundant in fruits, vegetables, lean proteins, and whole grains supports endothelial function and helps maintain healthy blood pressure levels. Specific dietary changes can also directly impact GERD symptoms, reducing acid reflux and minimizing vagal nerve stimulation.
Beyond the basic principles of heart-healthy eating, focusing on foods that promote vagal tone – the activity of the vagus nerve – can be beneficial. Foods rich in magnesium (leafy greens, nuts, seeds) and omega-3 fatty acids (fatty fish, flaxseeds, chia seeds) have been shown to support vagal nerve function. Conversely, highly processed foods and sugary drinks tend to suppress vagal tone. Additionally, mindful eating practices – slowing down during meals, chewing thoroughly, and paying attention to hunger cues – can also enhance vagal tone and improve digestive health. This holistic approach addresses both GERD and blood pressure concerns simultaneously. Planning dinner meals carefully is a good place to start. It’s worth considering whether there is a connection between GERD and hiccups.
It’s important to reiterate that the relationship between GERD and fluctuating blood pressure is complex and not fully understood. While physiological connections exist, establishing a direct cause-and-effect link remains challenging. Further research is needed to clarify these interactions and develop targeted management strategies.