Gastroesophageal reflux disease (GERD) is a surprisingly common condition, affecting millions worldwide. It’s often characterized by heartburn – that burning sensation in the chest – but its manifestations are far more diverse than many people realize. Beyond the typical symptoms, individuals with GERD frequently describe unusual sensations related to their esophagus, and one of the most perplexing is the feeling of sandpaper or grit within the esophageal passage. This isn’t simply discomfort; it’s a distinct textural sensation that can be incredibly unsettling and significantly impact quality of life. Understanding why this happens requires delving into the complexities of the digestive system, the mechanisms behind reflux, and how chronic inflammation plays a role in altered sensory perception.
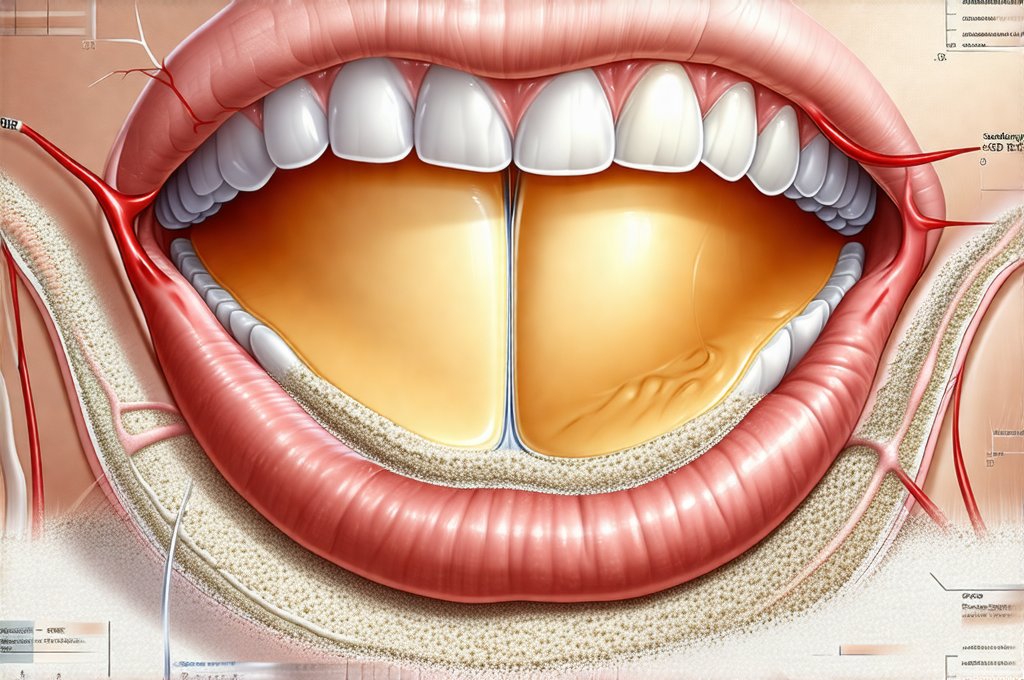
The esophagus is designed to swiftly transport food from your mouth to your stomach, but its delicate lining isn’t equipped to handle frequent exposure to stomach acid. When the lower esophageal sphincter (LES), the muscular valve separating the esophagus from the stomach, malfunctions or relaxes inappropriately, stomach contents – including acidic digestive juices – can flow back upwards. This reflux event is often what triggers heartburn, but it’s also what initiates a cascade of potential issues. The sandpaper feeling isn’t usually caused by actual physical abrasion; rather, it stems from inflammation and heightened sensitivity within the esophageal lining due to repeated acid exposure or other irritants. It represents a more subtle yet equally distressing symptom that warrants attention and understanding. Considering understanding the role of bile can provide further insight into reflux triggers.
Understanding Esophageal Sensitization
The sensation of sandpaper in the esophagus is often linked to esophageal hypersensitivity, sometimes referred to as visceral hypersensitivity. This isn’t about damage so much as it’s about the nervous system becoming overly sensitive to normal stimuli. Imagine a volume knob turned up too high on pain receptors within the esophageal lining. What might normally be a mild, unremarkable sensation is interpreted as intense and unpleasant. – Repeated acid exposure can lead to inflammation of the esophagus (esophagitis). – This inflammation damages nerve endings in the esophageal wall. – The nervous system then recalibrates itself, lowering the threshold for perceiving discomfort. Even normal digestive processes or mildly acidic reflux can trigger the sandpaper sensation because the sensitivity is increased.
This sensitization isn’t limited to acid. Other factors can contribute, including bile reflux (where bile from the small intestine flows back into the stomach and esophagus), food sensitivities, and even stress. The brain plays a crucial role too; chronic pain conditions often involve central sensitization, where the nervous system amplifies pain signals throughout the body. Essentially, the brain learns to perceive more discomfort, making individuals more reactive to stimuli that wouldn’t normally cause such a strong response. This explains why some people with GERD experience the sandpaper sensation even when objective tests don’t reveal significant inflammation – their sensitivity is the primary driver of the symptom. The role of FODMAPs may also be a contributing factor for some individuals.
The connection between psychological stress and esophageal hypersensitivity shouldn’t be underestimated. Stress can directly impact gut motility (the movement of food through the digestive system) and LES function, exacerbating reflux. It also influences pain perception pathways in the brain, amplifying discomfort. Managing stress through techniques like mindfulness, yoga, or therapy can sometimes provide significant relief for individuals experiencing this symptom. The role of yoga and physical therapy may offer benefits beyond IBS management as well.
Diagnostic Approaches & Testing
Pinpointing the cause of a sandpaper sensation requires careful evaluation by a healthcare professional. While self-diagnosis is never recommended, understanding the common diagnostic tools can empower you to have informed conversations with your doctor. – Endoscopy: This involves inserting a thin, flexible tube with a camera into the esophagus to visually inspect the lining for signs of inflammation or damage. Biopsies can be taken if necessary. – Esophageal Manometry: This test measures the pressure and coordination of muscle contractions within the esophagus, helping assess LES function and identify motility disorders. – pH Monitoring: This involves placing a small device in the esophagus to continuously monitor acid levels over 24-48 hours. It can reveal how often and for how long acid is refluxing into the esophagus.
It’s important to note that standard tests don’t always correlate with the intensity of symptoms experienced by patients with esophageal hypersensitivity. Someone may have relatively mild esophagitis on endoscopy but report intense discomfort. This highlights the importance of a comprehensive evaluation that considers both objective findings and subjective symptom reporting. Newer diagnostic techniques, such as impedance-pH monitoring (which detects both acid and non-acid reflux), can offer more insights into the specific triggers for an individual’s symptoms. Understanding the role of antacids in treatment is a good starting point, but diagnosis is crucial.
The interpretation of these tests is crucial. For instance, manometry might reveal a weak or relaxed LES, while pH monitoring could show frequent acid exposure. However, even with normal test results, the sandpaper sensation shouldn’t be dismissed. It suggests heightened sensitivity that needs to be addressed through alternative strategies (discussed later). The goal isn’t necessarily just to reduce acid production but also to recalibrate the nervous system and restore a more balanced sensory perception.
Lifestyle Modifications & Dietary Adjustments
Often, the first line of defense against GERD and related symptoms like the sandpaper sensation involves lifestyle modifications and dietary adjustments. These aren’t quick fixes, but they can significantly reduce reflux frequency and severity, potentially lessening esophageal sensitization over time. – Dietary Changes: Identify and eliminate trigger foods. Common culprits include fatty foods, spicy foods, chocolate, caffeine, alcohol, and carbonated beverages. Eating smaller, more frequent meals can also help. – Elevating the Head of Your Bed: Raising the head of your bed by 6-8 inches using blocks or a wedge pillow helps gravity keep stomach acid where it belongs. – Weight Management: Excess weight puts pressure on the abdomen, increasing the risk of reflux. Losing even a small amount of weight can make a difference. The role of weight management is essential for overall health.
Beyond these common recommendations, consider exploring strategies specifically aimed at reducing esophageal irritation. For example: 1. Chewing gum after meals stimulates saliva production, which helps neutralize stomach acid. 2. Staying hydrated throughout the day dilutes stomach acid and promotes digestive health. 3. Avoiding eating close to bedtime allows more time for digestion before lying down. The role of chewing gum provides a simple way to manage symptoms.
It’s essential to remember that dietary sensitivities are highly individual. What triggers symptoms in one person may not affect another. Keeping a food diary can help identify your personal trigger foods. Also, don’t drastically change your diet overnight. Gradual modifications are more sustainable and less likely to cause disruption. The focus should be on creating a long-term eating pattern that supports digestive health and minimizes reflux episodes. The importance of meal timing can also play a role in managing symptoms.
Pharmaceutical & Alternative Approaches
When lifestyle changes aren’t enough, medication may be necessary. – Antacids: Provide temporary relief by neutralizing stomach acid but don’t address the underlying cause of GERD. – H2 Blockers: Reduce acid production in the stomach. – Proton Pump Inhibitors (PPIs): More potent than H2 blockers and are often prescribed for severe GERD, but long-term use can have side effects.
However, relying solely on medication isn’t always ideal, especially for individuals with esophageal hypersensitivity. Addressing the underlying nerve sensitivity is crucial. Some promising alternative approaches include: – Visceral Pain Modulation: Techniques aimed at retraining the nervous system to reduce pain perception. This may involve biofeedback or cognitive behavioral therapy (CBT). – Probiotics: Emerging research suggests that certain probiotic strains can improve gut health and potentially reduce esophageal inflammation. – Mindfulness & Stress Reduction Techniques: As mentioned earlier, managing stress is vital for reducing both reflux and hypersensitivity.
It’s crucial to discuss any medication changes or alternative therapies with your healthcare provider before starting them. PPIs, while effective at suppressing acid, can sometimes paradoxically worsen esophageal hypersensitivity in the long run by altering the gut microbiome and potentially decreasing nerve function. A holistic approach that combines lifestyle modifications, targeted medications (when necessary), and strategies for addressing nerve sensitivity is often the most effective way to manage GERD and alleviate the distressing sensation of sandpaper in the esophagus. Remember that finding the right combination of treatments may take time and experimentation.