Endoscopic ultrasound (EUS) is a highly specialized medical procedure that combines endoscopy – visualizing internal organs with a camera on a flexible tube – with ultrasound technology. This powerful combination allows doctors to get detailed images of the digestive tract and nearby organs, including the pancreas, gallbladder, bile ducts, liver, stomach, duodenum, and even lungs in some cases. It’s not just about seeing these areas; EUS can also help guide biopsies, drain fluid collections, and deliver targeted therapies. This advanced diagnostic tool is becoming increasingly important for evaluating various gastrointestinal conditions and staging certain cancers, leading to more accurate diagnoses and treatment plans.
Unveiling the Power of Endoscopic Ultrasound
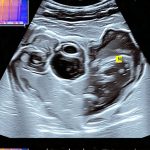
Endoscopic ultrasound isn’t a single test but rather a technique that uses a specialized endoscope—a long, thin, flexible tube with a camera and an ultrasound probe at its tip. Unlike traditional endoscopy which primarily visualizes the lining of the digestive tract, EUS allows doctors to visualize layers beneath the lining and adjacent structures not readily seen by conventional methods. This is achieved because the ultrasound probe emits high-frequency sound waves that create real-time images when they bounce back from different tissues. The endoscope is carefully guided through the mouth (or sometimes other natural openings) into the digestive tract, providing a clear view while simultaneously producing detailed ultrasound imagery. The resulting images are displayed on a monitor, allowing physicians to assess the size, shape, and structure of organs and detect abnormalities with remarkable precision. This technique has revolutionized how doctors diagnose and manage complex gastrointestinal conditions.
Why It’s Done: Identifying the Need for EUS
EUS is generally ordered when other less invasive tests haven’t provided enough information or when a doctor suspects a specific condition that requires more detailed evaluation. One of the most common applications is in the investigation of pancreatic cysts and masses, helping to determine whether they are benign or cancerous. It’s also used extensively in the diagnosis and staging of cancers of the esophagus, stomach, duodenum, pancreas, and bile ducts. Specifically, EUS with fine-needle aspiration (EUS-FNA) allows doctors to obtain a small tissue sample from suspicious areas for biopsy, providing critical information for accurate diagnosis and treatment planning.
Beyond cancer detection, EUS is invaluable in diagnosing conditions like:
* Chronic pancreatitis: Assessing the extent of inflammation and structural changes within the pancreas.
* Gallstones or blockages in the bile ducts: Identifying stones or tumors causing obstruction.
* Gastrointestinal bleeding: Locating the source of bleeding in the digestive tract.
* Inflammatory bowel disease (IBD): Evaluating the depth of inflammation and identifying complications.
* Esophageal strictures: Assessing narrowing of the esophagus.
EUS is often preferred over other imaging modalities like CT or MRI because it provides higher-resolution images of the gastrointestinal tract, minimizing radiation exposure, and allowing for real-time biopsy capabilities.
How to Prepare: Getting Ready for Your EUS Procedure
Preparation for an EUS procedure varies slightly depending on the specific reason for the test and the institution’s protocols. Generally, patients are asked to fast for at least six hours before the procedure – this ensures a clear view during examination and reduces the risk of aspiration (food or liquid entering the lungs) during sedation. You’ll need to inform your doctor about all medications you take, including over-the-counter drugs, vitamins, and supplements, as some may need to be adjusted or temporarily stopped before the test.
Here’s a typical pre-test checklist:
* Medication Review: Discuss all medications with your physician. Blood thinners might need adjustment.
* Fasting Requirements: Strictly adhere to fasting guidelines provided by your doctor. No solid food for at least six hours before the procedure, and liquids may also be restricted.
* Allergies: Inform your doctor of any allergies you have, especially to medications or latex.
* Transportation: Arrange for someone to drive you home after the procedure, as you will likely be sedated.
* Bowel Preparation: In some cases, a bowel preparation might be required – this involves drinking specific solutions to clear out the colon, which is particularly relevant if EUS is performed via the rectum (retroflex EUS).
Your doctor will provide detailed instructions tailored to your individual needs and medical history, so it’s vital to follow these carefully.
What to Expect During the Test: The Procedure Explained
The EUS procedure itself typically takes between 30 minutes to an hour, although this can vary based on the complexity of the exam and whether biopsies are performed. You’ll be asked to lie on your side (usually left side) while a qualified endoscopist performs the examination. Sedation is almost always administered intravenously to help you relax and minimize discomfort during the procedure. The level of sedation can range from moderate sedation, where you’re drowsy but still aware, to deeper sedation where you’re essentially asleep.
During the EUS:
1. The endoscope is gently inserted through your mouth (or other appropriate opening) and guided down into the digestive tract.
2. As the endoscope advances, the ultrasound probe emits sound waves, creating images of the surrounding tissues on a monitor.
3. If biopsies are needed (EUS-FNA), a fine needle is passed through the endoscope to collect tissue samples from suspicious areas. These samples are then sent to a laboratory for analysis.
4. In some cases, therapeutic interventions like fluid drainage or tumor ablation can be performed during EUS.
5. Throughout the procedure, your vital signs (heart rate, blood pressure, oxygen levels) will be closely monitored by healthcare professionals.
Understanding the Results: Interpreting What It Means
The results of an EUS examination are usually available relatively quickly, although it may take several days to receive biopsy results from the lab. The endoscopist will discuss initial findings with you immediately after the procedure. Images obtained during EUS provide valuable information about the size, location, and characteristics of any abnormalities detected within the digestive tract or surrounding organs.
What Your Test May Show:
- Benign vs. Malignant: Distinguishing between non-cancerous and cancerous growths.
- Stage of Cancer: Determining the extent of cancer spread (staging).
- Pancreatic Cyst Characteristics: Evaluating fluid content, wall thickness, and other features to assess risk of malignancy.
- Bile Duct Obstruction Cause: Identifying stones, tumors, or strictures causing blockage.
- Inflammation Depth: Assessing the severity of inflammation in conditions like IBD.
Biopsy results provide definitive diagnosis, confirming whether a mass is cancerous and identifying its specific type. EUS-FNA can also help guide treatment decisions, such as determining the best course of action for cancer therapy or managing chronic pancreatitis. Your doctor will explain the results clearly and answer any questions you may have.
Is It Safe? Risks and Side Effects
EUS is generally considered a safe procedure, but like all medical interventions, it carries some potential risks and side effects. Most are minor and temporary. Common side effects include:
* Sore throat: From the endoscope passing through the mouth.
* Bloating or gas: Due to air introduced during the procedure.
* Abdominal discomfort: Mild cramping or pain.
More serious, though rare, complications can include:
* Infection: From the biopsy site.
* Bleeding: From the biopsy site, usually minor and self-limiting.
* Pancreatitis: Inflammation of the pancreas (particularly after ERCP combined with EUS).
* Perforation: A very rare tear in the wall of the digestive tract.
* Adverse reaction to sedation: Including breathing difficulties or heart rate changes
Your healthcare team will take precautions to minimize these risks, and you should report any concerning symptoms after the procedure – such as fever, severe abdominal pain, persistent bleeding, or difficulty breathing – immediately.
Final Thoughts: A Powerful Diagnostic Tool
Endoscopic ultrasound is a sophisticated diagnostic tool offering invaluable insights into the digestive system and surrounding organs. It goes beyond traditional imaging methods to provide detailed visualizations, guide biopsies with precision, and even facilitate targeted therapies. While it’s not without potential risks, these are generally minimal, making EUS a powerful ally in diagnosing and managing a wide range of gastrointestinal conditions. The ability to accurately stage cancers and evaluate complex pancreatic diseases has significantly improved patient care and treatment outcomes.
Questions about this test? Drop them in the comments and we’ll respond.