Chronic fatigue—that persistent, draining lack of energy—afflicts millions. Often, we look for quick fixes: more coffee, stricter schedules, even pushing through despite exhaustion. But what if the root cause isn’t a willpower issue, but something deeper within our bodies? Increasingly, research points to the gut as a surprisingly powerful player in overall energy levels. It’s not simply about digestion; it’s about a complex ecosystem that impacts everything from nutrient absorption to immune function and even mental wellbeing – all critical components of sustained vitality. Ignoring this internal world can leave us perpetually running on empty, chasing symptoms instead of addressing the source. Considering compassion practices might also be beneficial in navigating these challenges.
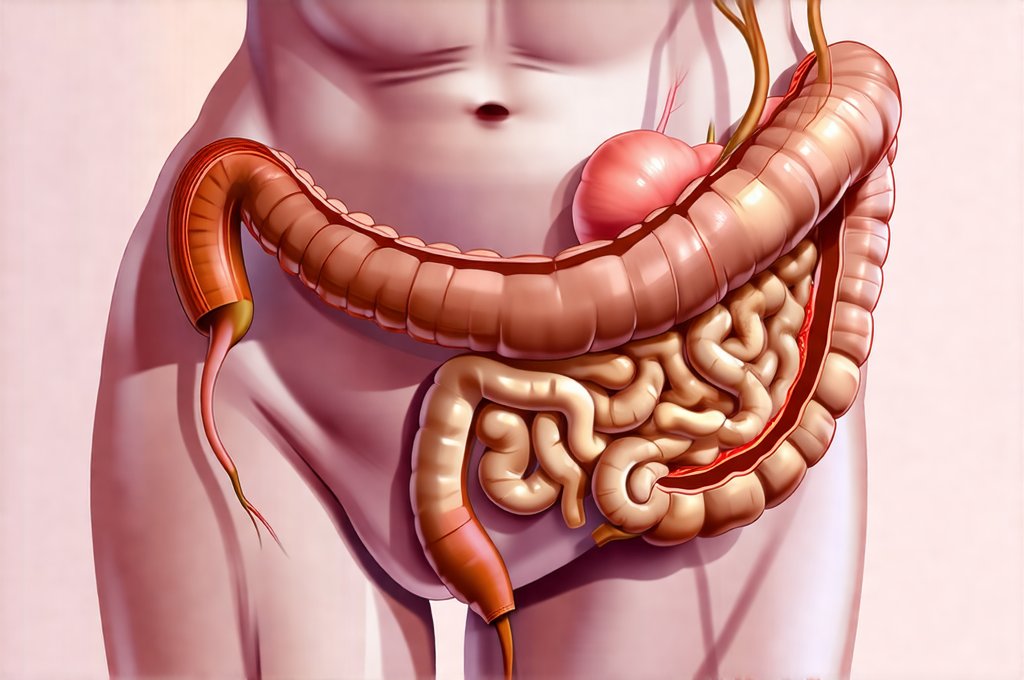
The gut’s influence extends far beyond processing food. It’s home to trillions of microorganisms – bacteria, viruses, fungi, and archaea – collectively known as the gut microbiome. This diverse community isn’t just passively residing within us; it actively participates in our health. They help digest foods we can’t break down ourselves, synthesize essential vitamins (like K and B vitamins), regulate inflammation, and even communicate with the brain via what’s called the gut-brain axis. A disrupted microbiome—an imbalance known as dysbiosis—can lead to a cascade of issues that directly contribute to low energy, including impaired nutrient absorption, increased inflammation, and compromised immune function. Understanding this intricate relationship is crucial for reclaiming sustained energy levels. Prioritizing sleep tips can also improve your microbiome health.
The Gut-Energy Connection: How It Works
The link between gut health and energy isn’t always obvious, but it’s profoundly impactful. Think of your food as fuel – not just for physical activity, but also for all the cellular processes that keep us alive. If your gut isn’t efficiently absorbing nutrients from food, you’re essentially running on a depleted tank. This can happen due to several factors linked to gut dysfunction: – Reduced digestive enzyme production – Inflammation damaging the intestinal lining – Imbalances in gut bacteria affecting nutrient uptake. Beyond nutrient absorption, the gut microbiome directly impacts energy production at the cellular level. Mitochondria, often called the powerhouses of our cells, require specific nutrients to function optimally. A compromised gut hinders their ability to generate adequate ATP (adenosine triphosphate), the primary energy currency of the body. You might find how to eat for energy helpful in optimizing this process.
Furthermore, chronic inflammation—often originating in the gut—is a significant energy drain. When the immune system is constantly activated due to gut dysbiosis or leaky gut (increased intestinal permeability), it diverts resources from other essential functions, leaving you feeling fatigued and depleted. The gut-brain axis also plays a role. An unhealthy gut can disrupt neurotransmitter production—chemicals that regulate mood, sleep, and energy levels. For example, serotonin, often called the “happy hormone,” is largely produced in the gut. Imbalances here can contribute to fatigue, low motivation, and even depression, creating a vicious cycle of low energy. A healthy gut isn’t just about what you eat; it’s about how well your body utilizes what you consume. Considering calming flavor profiles can also help reduce inflammation.
Restoring Gut Function: Practical Steps
Restoring gut function is rarely a quick fix, but it’s achievable with consistent effort and a holistic approach. It’s often about creating an environment where beneficial bacteria can thrive while minimizing factors that disrupt the microbiome. Dietary changes are paramount, focusing on nourishing foods that support gut health. This includes: – A diverse range of fiber-rich fruits and vegetables – fiber feeds beneficial bacteria – Fermented foods like yogurt (with live cultures), kefir, sauerkraut, and kimchi – these introduce probiotics directly into the gut – Healthy fats from sources like avocado, olive oil, and fatty fish – essential for overall health and nutrient absorption. Equally important is identifying and eliminating food sensitivities that contribute to inflammation. Common culprits include gluten, dairy, soy, and processed foods. An elimination diet, guided by a healthcare professional, can help pinpoint these triggers.
Beyond diet, lifestyle factors play a significant role. Managing stress levels is crucial, as chronic stress negatively impacts gut health. Incorporating practices like mindfulness, yoga, or spending time in nature can significantly reduce stress hormones that disrupt the microbiome. Prioritizing sleep is also essential; adequate rest allows the body to repair and regenerate, including the gut lining. Finally, consider incorporating prebiotics – foods that feed beneficial bacteria – into your diet. Examples include garlic, onions, asparagus, and bananas. Remember, restoration isn’t about perfection; it’s about progress. Small, sustainable changes are more effective than drastic overhauls. If you have GERD, explore best dairy alternatives for a gut-friendly diet.
Identifying Potential Gut Issues
Pinpointing the specific gut issues contributing to low energy can be challenging, as symptoms often overlap with other conditions. However, certain signs may indicate a deeper problem. These include: – Persistent bloating and gas – Frequent heartburn or acid reflux – Changes in bowel habits (diarrhea, constipation, or both) – Food sensitivities – experiencing discomfort after eating specific foods – Skin issues like eczema or acne – gut health is often linked to skin health. While these symptoms don’t definitively diagnose a gut problem, they warrant further investigation.
A comprehensive stool test can provide valuable insights into the composition of your microbiome and identify imbalances or pathogens. This test can reveal levels of beneficial bacteria, potential infections, and markers of inflammation. Working with a healthcare professional knowledgeable about functional medicine or gastroenterology is crucial for interpreting these results accurately and developing a personalized treatment plan. It’s important to note that self-diagnosis can be misleading, and professional guidance ensures you’re addressing the underlying issues effectively. Don’t dismiss persistent gut symptoms; they are often signals from your body needing attention.
The Role of Leaky Gut Syndrome
Leaky gut syndrome, also known as increased intestinal permeability, is a condition where the lining of the small intestine becomes damaged, allowing undigested food particles, toxins, and bacteria to escape into the bloodstream. This triggers an immune response, leading to chronic inflammation which, as previously discussed, drains energy levels. While still debated within mainstream medicine, many functional medicine practitioners believe leaky gut plays a significant role in various health conditions, including fatigue.
Factors contributing to leaky gut include: – A diet high in processed foods, sugar, and unhealthy fats – Chronic stress – Antibiotic use – which can disrupt the microbiome – Certain medications like NSAIDs (nonsteroidal anti-inflammatory drugs). Addressing leaky gut typically involves removing trigger foods, restoring gut bacteria with probiotics and prebiotics, and incorporating nutrients that support intestinal repair. L-glutamine, an amino acid, is often recommended to help heal the gut lining. It’s important to remember that addressing leaky gut isn’t about simply “sealing” the gut; it’s about restoring overall gut health.
Supplementation: A Supporting Role
While diet and lifestyle are foundational for gut health, supplementation can sometimes provide targeted support. Probiotics—live microorganisms—can help repopulate the gut with beneficial bacteria. However, choosing the right probiotic is crucial. Different strains have different effects, so it’s best to consult with a healthcare professional to determine which one is appropriate for your specific needs. Prebiotic supplements – like inulin or FOS (fructooligosaccharides) – can nourish existing beneficial bacteria and promote their growth.
Digestive enzymes can aid in breaking down food, improving nutrient absorption and reducing digestive discomfort. L-glutamine, as mentioned earlier, supports intestinal repair. However, supplementation should never replace a healthy diet and lifestyle. It’s best to view supplements as tools to complement these foundational elements, not as standalone solutions. Always consult with a healthcare professional before starting any new supplement regimen. They can help you determine the appropriate dosage, potential interactions, and whether supplementation is right for you. Prioritizing whole foods and addressing underlying lifestyle factors remains paramount for sustained energy and overall wellbeing. Learning best cooking methods can support gut health through food preparation too. Finally, remember the benefits of eating mindfully.