Digestive health is often an overlooked component of overall well-being, yet it profoundly impacts everything from nutrient absorption and immune function to mental clarity and energy levels. For many years, annual checkups primarily focused on cardiovascular health, blood pressure, and basic metabolic markers. However, there’s a growing recognition that a proactive approach to digestive health is essential for preventative care, leading to the increasing inclusion of specialized digestive health panels in routine examinations. This shift reflects a deeper understanding of the gut-brain axis – the bidirectional communication system between the digestive tract and the brain – and its influence on systemic health.
Traditionally, concerns about digestion were addressed only when symptoms like bloating, abdominal pain, or changes in bowel habits arose. Now, healthcare providers are realizing that identifying subtle imbalances before noticeable issues occur can prevent chronic conditions and improve quality of life. Digestive health panels aren’t merely diagnostic tools; they represent a move towards personalized preventative medicine, allowing for tailored dietary recommendations, lifestyle adjustments, and targeted interventions to optimize gut function. The goal is not just the absence of disease but the active promotion of digestive wellness as an integral part of holistic health.
Emerging Trends in Digestive Health Panels
The composition of these panels has evolved significantly over time. Early iterations might have included only basic stool tests checking for occult blood or parasitic infections. Modern panels are far more comprehensive, incorporating advanced technologies like microbiome sequencing and functional stool analysis to provide a granular understanding of gut ecosystem dynamics. This increased sophistication allows for the identification of underlying causes of digestive distress rather than simply treating symptoms. The inclusion of markers related to inflammation, nutrient absorption, and intestinal permeability is also becoming increasingly common.
The rise in chronic diseases – autoimmune disorders, allergies, obesity, and even mental health conditions – has fueled this demand for more detailed digestive assessments. Research consistently demonstrates a strong link between gut dysbiosis (an imbalance in the gut microbiome) and these illnesses. By identifying imbalances early on, healthcare professionals can implement strategies to restore gut balance and potentially mitigate the risk of developing or worsening chronic ailments. Furthermore, personalized nutrition plans based on individual microbiome profiles are gaining traction as an effective means of optimizing digestive health and overall well-being. Understanding how role of enzymes impacts the body is key to this process.
These panels are becoming more accessible too. While previously reserved for patients with diagnosed gastrointestinal issues, they’re now being offered as part of standard annual checkups at many progressive healthcare facilities. This accessibility, combined with increased public awareness about the importance of gut health, is driving further demand and innovation in the field. The integration of telehealth and home testing kits also contributes to ease of access. Considering fermented foods can also play a part in improving gut health.
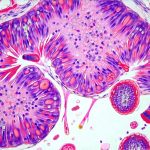
Understanding Microbiome Sequencing
Microbiome sequencing represents a revolutionary advancement in digestive health assessment. It goes beyond identifying which bacteria are present in the gut; it quantifies their abundance, assesses diversity, and reveals potential imbalances that could contribute to health problems. Traditionally, bacterial cultures were used to identify microorganisms, but they only capture organisms that can be easily grown in a lab – missing a significant portion of the microbiome’s complexity. Sequencing allows for a much more comprehensive picture.
- The process typically involves collecting a stool sample and sending it to a specialized laboratory.
- There, DNA is extracted from the sample and analyzed using advanced sequencing technologies.
- Results are then compared to reference databases to identify the types and quantities of microorganisms present.
The information gleaned from microbiome sequencing can inform personalized dietary recommendations (e.g., increasing fiber intake to promote beneficial bacteria), probiotic or prebiotic supplementation strategies, and lifestyle modifications aimed at restoring gut balance. It’s important to note that a “healthy” microbiome isn’t defined by the presence of specific organisms but rather by its diversity and relative abundance of different microbial groups. A diverse microbiome is generally more resilient and better equipped to withstand disruptions. For further information on how your body processes food, review apple cider vinegar.
Functional Stool Analysis: Beyond Identification
While microbiome sequencing identifies who lives in the gut, functional stool analysis reveals what they are doing. It assesses various metabolic markers that indicate how well the digestive system is functioning – things like levels of short-chain fatty acids (SCFAs), pancreatic elastase, and inflammatory markers. SCFAs, produced by bacterial fermentation of fiber, are crucial for gut health and overall inflammation regulation. Low SCFA levels may suggest insufficient fiber intake or an imbalance in the microbiome.
Pancreatic elastase is a marker of exocrine pancreatic function – the pancreas’ ability to produce digestive enzymes. Reduced levels can indicate pancreatic insufficiency, leading to malabsorption of nutrients. Markers of inflammation, such as calprotectin and lactoferrin, can signal underlying gut inflammation, which may be indicative of conditions like inflammatory bowel disease (IBD). Functional stool analysis provides a more holistic assessment of digestive function compared to microbiome sequencing alone, offering insights into the overall health of the gastrointestinal tract. Proper digestive enzymes are vital for breaking down food effectively.
Intestinal Permeability (“Leaky Gut”) Assessment
The concept of “leaky gut” – or increased intestinal permeability – has gained considerable attention in recent years. It refers to a condition where the tight junctions between cells lining the intestinal wall become compromised, allowing undigested food particles, toxins, and bacteria to leak into the bloodstream. This can trigger an immune response and contribute to systemic inflammation. Assessing intestinal permeability is becoming more common within digestive health panels, although it’s often a controversial topic.
Several methods are used to assess intestinal permeability:
1. Lactulose/mannitol test: Involves consuming these sugars and measuring their excretion in urine; higher lactulose excretion suggests increased permeability.
2. Zonulin levels: Zonulin is a protein that regulates tight junctions; elevated levels may indicate increased permeability.
It’s important to understand that intestinal permeability isn’t necessarily a disease itself but rather a functional abnormality that can contribute to various health problems. Addressing factors that increase permeability – such as chronic stress, poor diet, and certain medications – is crucial for restoring gut health. However, interpreting these tests requires caution, as results can be influenced by numerous variables. Understanding the role of synbiotics in maintaining a healthy balance can also be beneficial.
The inclusion of digestive health panels in annual checkups represents a significant step forward in preventative healthcare. By moving beyond traditional symptom-based approaches and embracing proactive assessments of gut function, we can empower individuals to take control of their digestive wellness and optimize their overall health. As research continues to unravel the complexities of the gut microbiome and its impact on systemic health, these panels are likely to become even more sophisticated and integral to routine medical care. Keeping mucosal health in check can also improve overall digestive function. And don’t forget about the importance of gallbladder health.