The esophagus, often called the food pipe, is a vital component of our digestive system, responsible for safely transporting food from the mouth to the stomach. It’s a remarkably resilient organ, but constant exposure to acidic foods, certain lifestyle choices, and underlying conditions can gradually take their toll, leading to issues like heartburn, acid reflux (GERD), Barrett’s esophagus, and even esophageal cancer in severe cases. Many people only think about esophageal health when symptoms arise, but adopting preventative daily habits is far more effective than reactive treatment. Protecting this crucial part of your digestive system isn’t a complex undertaking; it’s largely about making informed choices that support its natural function and minimize stress.
This article will explore practical, everyday adjustments you can make to safeguard your esophageal health long-term. We’ll delve into dietary considerations, lifestyle modifications, and behavioral changes—all designed to create a proactive approach to esophageal well-being. It’s important to understand that these habits aren’t about deprivation or strict rules; they are about cultivating mindful practices that support overall digestive health and minimize the risk of future complications. The goal is not just symptom management but prevention through consistent, positive choices.
Dietary Strategies for Esophageal Health
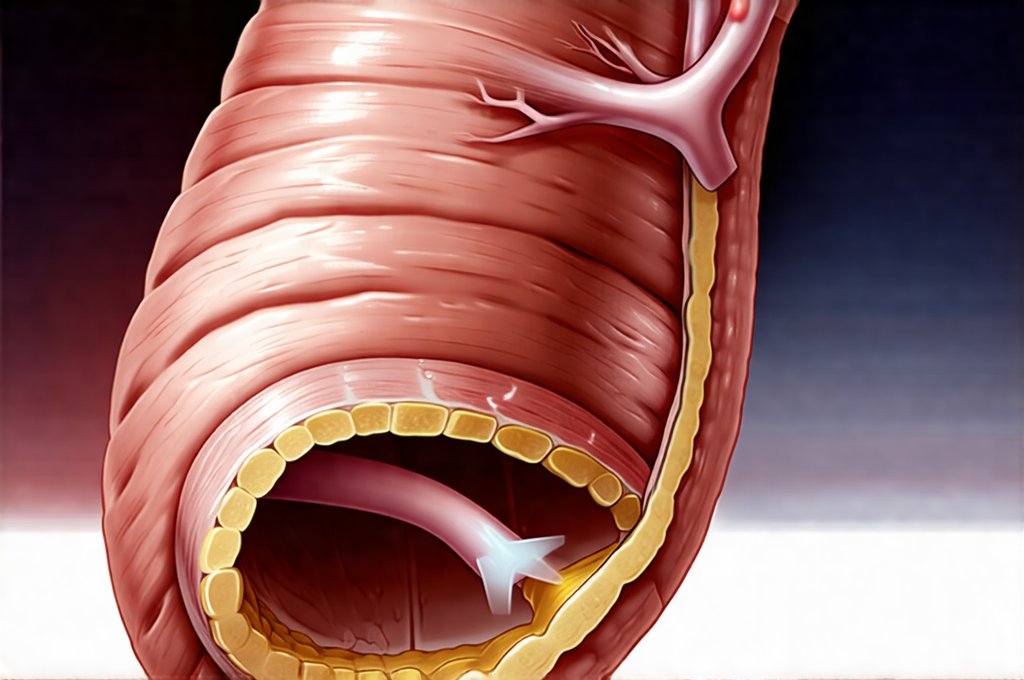
The food we consume plays a significant role in esophageal health, directly impacting acidity levels and potential irritation. Certain foods can exacerbate symptoms or contribute to long-term damage, while others actively support a healthy digestive process. Focusing on whole, unprocessed foods is generally the best starting point. A diet rich in fiber helps maintain regularity and reduces pressure within the abdomen, lessening the likelihood of acid reflux. Conversely, high-fat foods, spicy dishes, chocolate, caffeine, carbonated beverages, and alcohol can all relax the lower esophageal sphincter (LES), allowing stomach acid to flow back up into the esophagus.
Understanding trigger foods is incredibly important; what causes discomfort for one person might not affect another. Keeping a food diary to track your meals and associated symptoms can be an invaluable tool in identifying personal sensitivities. This isn’t about eliminating all “bad” foods forever, but rather being mindful of portion sizes and frequency. For example, enjoying a small piece of dark chocolate occasionally is unlikely to cause significant issues for most people, while regularly indulging in large quantities could contribute to reflux.
Beyond avoiding trigger foods, incorporating esophageal-friendly options can be highly beneficial. Foods rich in alkaline properties – like bananas, melons, and leafy greens – may help neutralize stomach acid. Drinking plenty of water throughout the day aids digestion and helps dilute stomach acids. Furthermore, smaller, more frequent meals are generally easier on the esophagus than large portions, which increase pressure within the abdomen and the risk of reflux. Prioritizing lean proteins, complex carbohydrates, and healthy fats ensures a balanced diet that supports overall digestive health without overwhelming the esophageal system. Supporting enzyme efficiency through dietary choices is also key to optimal digestion.
Optimizing Meal Timing & Portion Control
Meal timing is often overlooked but can have a significant impact on esophageal health. Eating large meals close to bedtime increases the likelihood of acid reflux during sleep because the body’s natural clearing mechanisms are less efficient when lying down. Ideally, finish eating at least 2-3 hours before going to bed. This allows sufficient time for digestion and reduces the chance of nighttime discomfort. Similarly, avoid lying down immediately after eating; remain upright for a period to allow gravity to assist with the digestive process.
Portion control is another key element. Overeating stretches the stomach, increasing pressure on the LES and promoting reflux. It’s far more effective to eat smaller, more frequent meals throughout the day than to consume three large meals. This approach helps maintain consistent digestion and minimizes stress on the esophageal system. Consider using smaller plates and bowls to visually cue portion control, and practice mindful eating—paying attention to your body’s hunger and fullness cues.
Finally, chewing food thoroughly is paramount. Proper mastication breaks down food into smaller particles, reducing the workload for the stomach and esophagus. It also stimulates saliva production, which contains enzymes that begin the digestive process and help neutralize stomach acid. Taking your time during meals and focusing on chewing each bite properly can significantly improve digestion and reduce esophageal irritation. You might be surprised by how chewing habits impact overall comfort!
The Role of Hydration & Fiber
Staying adequately hydrated is essential for overall health, but it’s particularly important for esophageal well-being. Water helps dilute stomach acids, reducing their corrosive potential. It also aids in the smooth passage of food through the digestive tract, minimizing the risk of blockages or irritation. Aim to drink at least eight glasses of water daily, and increase your intake if you are physically active or live in a hot climate. Avoid substituting sugary drinks or caffeinated beverages for water, as these can actually exacerbate esophageal problems. Daily habits that support digestive comfort extend to staying well-hydrated.
Fiber plays a crucial role in digestive health and indirectly supports the esophagus. Dietary fiber adds bulk to stool, promoting regularity and reducing constipation. Constipation increases abdominal pressure, which can contribute to acid reflux. A high-fiber diet also slows down digestion, giving your stomach more time to process food properly before it reaches the esophagus. Good sources of fiber include fruits, vegetables, whole grains, legumes, and nuts. Gradually increase your fiber intake to avoid bloating or gas, and always drink plenty of water to help move the fiber through your digestive system.
Identifying & Limiting Trigger Foods
As mentioned earlier, identifying individual trigger foods is vital for proactive esophageal health. Common culprits include: – Citrus fruits and juices – Tomatoes and tomato-based products – Spicy foods – Chocolate – Caffeine (coffee, tea, soda) – Alcohol – Peppermint – While seemingly benign, peppermint can relax the LES. Keeping a detailed food diary where you log what you eat, when you eat it, and any associated symptoms is an excellent starting point.
Be specific in your logging—note not just what you ate but also the portion size and how you felt afterward. Look for patterns over time to identify foods that consistently trigger heartburn or other esophageal discomfort. Once identified, don’t necessarily eliminate these foods entirely; instead, focus on limiting their consumption and observing how smaller portions affect your symptoms. It’s also important to remember that seemingly innocuous combinations can sometimes be problematic. For example, a spicy meal paired with a carbonated beverage might cause more significant issues than either food individually. Understanding how pancreatic and enzymatic function relates to trigger foods is also helpful. Creating rituals that help when your gut feels unsafe can provide comfort during flare-ups. A healthy liver is essential for digestion, so consider incorporating habits from how to build a daily routine. Finally, remember that developing regular bowel rhythm supports overall digestive health.