The gut microbiome – trillions of bacteria, fungi, viruses, and other microorganisms residing in our digestive tract – has emerged as a central player in overall health. It’s no longer simply about digestion; we now understand the profound influence this ecosystem has on immunity, mental wellbeing, hormone regulation, even chronic disease risk. However, assessing gut health isn’t straightforward. A single test rarely provides the comprehensive understanding needed to address individual needs effectively. Relying solely on symptom evaluation or basic stool testing can paint an incomplete picture, potentially leading to misdirected interventions.
Traditional approaches often focus on identifying obvious issues like bacterial imbalances (dysbiosis) or digestive enzyme deficiencies. While valuable, these are just pieces of a larger puzzle. The gut is incredibly complex and dynamic; its composition changes constantly based on diet, lifestyle, stress levels, medications, and countless other factors. A truly insightful assessment requires looking beyond surface-level markers and considering the interplay between different microbial communities, their metabolic products, and host interactions. This means combining multiple testing methods to build a holistic understanding of an individual’s unique gut ecosystem.
The Landscape of Gut Testing Options
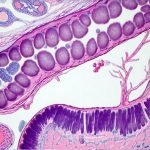
The market for gut health testing has exploded in recent years, offering a wide range of options with varying levels of accuracy, cost, and complexity. Understanding the different approaches is crucial for selecting tests that align with specific goals and concerns. Broadly, these can be categorized into stool tests, breath tests, blood tests, and emerging technologies like microbiome sequencing. Stool tests are currently the most accessible and commonly used method, analyzing microbial composition (identifying bacteria, fungi, etc.), metabolic markers (short-chain fatty acids, calprotectin), and indicators of digestion and absorption. Breath tests assess gut fermentation patterns and can help diagnose conditions like Small Intestinal Bacterial Overgrowth (SIBO). Blood tests primarily evaluate intestinal permeability (“leaky gut”) and inflammatory markers but provide limited information on the microbiome itself.
The rise of next-generation sequencing (NGS) has revolutionized our ability to analyze the microbiome with unprecedented detail. NGS technologies, often used in stool samples, identify the vast diversity of microorganisms present, providing a comprehensive snapshot of microbial communities. However, it’s important to note that even NGS data requires careful interpretation – identifying bacteria is only part of the story; understanding their function and interactions is equally vital. Simply knowing what microbes are present doesn’t necessarily tell you how they’re impacting health. It’s also crucial to recognize that testing isn’t an end in itself. The goal is not just data, but actionable insights that can inform targeted interventions.
Combining tests allows us to validate findings and get a more nuanced picture of gut function. For example, a stool test might reveal low levels of Bifidobacteria, while a breath test confirms SIBO. This suggests the reduced Bifidobacteria may be due to competition from overgrown bacteria in the small intestine. Or, blood tests showing elevated intestinal permeability alongside specific microbial imbalances in a stool analysis could point towards a compromised gut barrier contributing to systemic inflammation.
Building a Comprehensive Gut Health Assessment
The ideal combination of tests depends on an individual’s symptoms and health history, but some general strategies can be applied. A foundational approach often starts with a comprehensive stool test that includes: – Microbial identification (bacteria, fungi, archaea) – Metabolic marker analysis (SCFA, bile acids, pancreatic elastase) – Inflammation markers (calprotectin, lactoferrin) – Indicators of digestion and absorption
This provides a baseline understanding of the microbiome’s composition, digestive function, and inflammatory status. However, this is rarely enough on its own. To further refine the assessment, consider adding tests that address specific areas of concern or potential imbalances. For example: 1. SIBO Breath Test: If bloating, gas, or abdominal discomfort are prominent symptoms, a breath test can help determine if SIBO is present. 2. Intestinal Permeability Assessment (Blood): For individuals with autoimmune conditions, food sensitivities, or chronic fatigue, assessing intestinal permeability can identify a potential driver of systemic inflammation. 3. Organic Acids Test (Urine): This assesses metabolic function and can reveal deficiencies in essential nutrients or imbalances in gut microbial activity.
The key is to move beyond single data points and look for correlations between different test results. A stool test might show an abundance of a specific bacteria known to produce histamine, but without also assessing histamine reaction or looking at symptoms of histamine intolerance, it’s difficult to determine if this bacterial activity is contributing to health problems. Furthermore, remember that testing provides information, not diagnoses. It’s essential to work with a healthcare professional who can interpret the results within the context of your individual circumstances and develop a personalized plan. You may even need to reset your gut afterward.
Interpreting Results & Actionable Steps
Once you have a collection of test results, the real work begins: interpretation. This is where the expertise of a qualified practitioner is invaluable. Raw data from microbiome sequencing or stool tests can be overwhelming; a skilled professional can help identify patterns, prioritize findings, and translate them into actionable steps. It’s crucial to avoid falling into the trap of chasing individual microbes or obsessing over “good” versus “bad” bacteria. The microbiome is a complex ecosystem where balance and diversity are more important than eliminating specific organisms.
Interventions should be tailored to address underlying imbalances rather than simply targeting symptoms. For example, if SIBO is diagnosed alongside low levels of beneficial bacteria in the stool, treatment might involve addressing the bacterial overgrowth (with herbal antimicrobials or dietary changes) and supporting microbiome restoration with probiotics, prebiotics, and a gut-healing diet. Dietary modifications are often the cornerstone of any gut health plan. This may include eliminating inflammatory foods, increasing fiber intake to support beneficial bacteria, incorporating fermented foods to introduce probiotic strains, and optimizing hydration. If you’re looking for ways to optimize your diet, consider how to plan a menu that supports gut health.
Finally, remember that gut health is an ongoing process – it’s not about achieving a “fixed” state but rather cultivating a resilient and adaptable ecosystem. Regular monitoring, lifestyle adjustments, and continued attention to diet and stress management are essential for long-term wellbeing. Focusing on holistic strategies—nutrition, stress reduction, sleep optimization, and mindful movement—will yield far greater benefits than solely focusing on test results or chasing the latest gut health trend. You might even consider a gentle cleanse to support your efforts at rebuilding a diverse microbiome. Don’t forget that you can still enjoy spices even with a sensitive gut!