The digestive system, often referred to as “the gut,” is an incredibly complex network responsible for breaking down food, absorbing nutrients, and eliminating waste. When something goes awry within this intricate system, it can manifest in a wide range of uncomfortable—and sometimes serious—symptoms. From bloating and abdominal pain to changes in bowel habits and nausea, pinpointing the source of these issues can be challenging. Many people understandably turn to medical imaging as a means of understanding what’s happening inside their bodies, and among the various options available, the abdominal ultrasound is frequently considered due to its non-invasive nature and relative affordability. However, the question remains: just how much can an abdominal ultrasound reveal about your gut’s health?
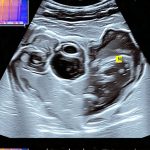
An abdominal ultrasound uses sound waves to create images of the organs within the abdomen, including those directly involved in digestion like the stomach, intestines, liver, gallbladder, pancreas, and spleen. It’s a valuable diagnostic tool, but it’s important to understand its strengths and limitations. While excellent at visualizing certain structures and detecting specific abnormalities, an ultrasound isn’t always able to provide a complete picture of everything going on within the gut. The clarity of images can also be affected by factors like body habitus (size/shape) and the presence of gas in the intestines. This article will delve into what abdominal ultrasounds can show about your gut, what they aren’t as effective at detecting, and how this imaging modality fits within a broader diagnostic approach.
What an Abdominal Ultrasound Can Detect
An abdominal ultrasound excels at visualizing several key aspects of the digestive system, making it a useful first-line investigation for many gastrointestinal complaints. It’s particularly good at identifying issues related to solid organs connected to digestion and can offer valuable information about fluid collections within the abdomen. For example, gallstones—a common cause of upper abdominal pain—are easily identified with ultrasound because they create strong reflections of sound waves. Similarly, abnormalities in the liver, such as cysts or tumors (though further investigation is usually needed), can often be detected.
The pancreas, which plays a vital role in digestion and blood sugar regulation, is another organ well-suited for ultrasound evaluation. Inflammation of the pancreas (pancreatitis) or the presence of pancreatic cysts can frequently be visualized using this technique. The spleen, while not directly involved in digestion, sits nearby and can also be assessed for size, shape, and any signs of injury or disease. Furthermore, an abdominal ultrasound is useful in detecting fluid accumulation around the intestines (ascites), which may indicate underlying problems like infections or cancers. Importantly, it’s a relatively quick and painless procedure, requiring no radiation exposure – making it safe for most individuals, including pregnant women.
Ultrasound can also be used to assess blood flow within these organs. Doppler ultrasound, a specialized type of ultrasound, allows doctors to evaluate the velocity and direction of blood moving through arteries and veins, helping identify potential blockages or narrowing that could compromise organ function. This is especially useful in assessing for conditions like mesenteric ischemia (reduced blood flow to the intestines). It’s important to remember though, that while it can show evidence of reduced blood flow, it doesn’t always pinpoint the exact cause.
Identifying Specific Gut Issues with Ultrasound
While an ultrasound isn’t a perfect tool for directly visualizing the intestines themselves (due to gas interference as mentioned earlier), it can detect secondary signs indicating problems within them. – Inflammation around the intestinal walls may be visible as thickening or fluid buildup. – Abscesses, collections of pus caused by infection, are often readily identified. – Bowel obstruction can sometimes be suggested by dilated loops of bowel – meaning they’re stretched out due to blockage – although other imaging modalities are generally preferred for definitive diagnosis.
Furthermore, ultrasound is helpful in guiding procedures like paracentesis (removing fluid from the abdomen) or biopsies. This allows doctors to accurately target specific areas for sample collection with increased precision and reduced risk. It’s also important to note that an abdominal ultrasound can often differentiate between a fluid-filled cyst and a solid mass, which helps narrow down potential diagnoses. However, it’s rarely definitive on its own; further investigations are usually required to confirm the nature of any detected abnormalities. If you suspect your gut is struggling with transit time, consider signs indicating issues.
Limitations & Complementary Tests
Despite its benefits, an abdominal ultrasound has significant limitations when it comes to evaluating the gut. The presence of gas within the intestines creates a “shadowing” effect, obscuring deeper structures and making it difficult to visualize the bowel wall clearly. This makes it challenging to detect subtle abnormalities like small polyps or early-stage cancers within the colon. Similarly, ultrasound struggles with visualizing the entire length of the small intestine due to its complex anatomy and frequent gas pockets.
Because of these limitations, an abdominal ultrasound is often used in conjunction with other diagnostic tests. – CT scans (computed tomography) provide more detailed cross-sectional images and are better at visualizing the intestines, but involve radiation exposure. – MRI scans (magnetic resonance imaging) offer even greater detail and don’t use radiation, but they’re more expensive and time-consuming. – Endoscopy/Colonoscopy allows direct visualization of the intestinal lining and enables biopsies to be taken – often considered the gold standard for diagnosing many gut conditions. – Stool tests can help identify infections or inflammation within the digestive tract.
The choice of which test(s) to use depends on your specific symptoms, medical history, and what your doctor suspects is causing your problems. An ultrasound might be a starting point, but it’s rarely the final answer. Understanding immune cycles can also help you understand your overall health picture.
The Role in Diagnostic Pathways
An abdominal ultrasound frequently serves as an initial screening tool when someone presents with abdominal pain, bloating, nausea, or changes in bowel habits. It’s often ordered before more advanced (and potentially costly) imaging studies like CT scans or MRIs are considered, helping to rule out certain conditions quickly and efficiently. For instance, if a patient complains of right upper quadrant pain, an ultrasound can rapidly assess for gallstones, which is a common cause of this symptom. If the ultrasound is normal, it reduces the likelihood of gallbladder-related issues and prompts the doctor to investigate other possibilities.
However, relying solely on an abdominal ultrasound can lead to missed diagnoses or delays in treatment. The limitations regarding intestinal visualization mean that conditions like Crohn’s disease (chronic inflammatory bowel disease) are often difficult to detect with ultrasound alone – requiring endoscopy/colonoscopy for confirmation. Similarly, subtle tumors within the colon might go unnoticed. Therefore, it’s crucial for patients and doctors to understand the nuances of this imaging modality and interpret its findings carefully. A “normal” ultrasound doesn’t necessarily mean there’s nothing wrong; it simply means that no obvious abnormalities were detected with this method. Building a tolerant gut can play an important role in long-term health.
The diagnostic pathway often involves a combination of clinical assessment (patient history, physical exam), blood tests, stool tests, imaging studies (including ultrasound), and potentially endoscopic procedures to arrive at an accurate diagnosis. The doctor will consider all available information to determine the most appropriate course of action, which might include medication, lifestyle changes, or further investigations. Ultimately, an abdominal ultrasound is one piece of the puzzle, not the entire solution.
Understanding Ultrasound Reports
Receiving and understanding your ultrasound report can be daunting. It’s often filled with medical jargon that’s difficult to decipher. Here are some key terms you might encounter: – Echogenic: Describes areas that reflect sound waves strongly, appearing bright on the image. – Hypoechoic: Describes areas that reflect sound waves weakly, appearing darker on the image. – Anechoic: Describes areas that don’t reflect sound waves at all, appearing completely black (often indicating fluid-filled structures).
The report will typically describe the size, shape, and location of organs, as well as any abnormalities detected. It may also include measurements, such as the diameter of a gallstone or the thickness of an intestinal wall. Importantly, the radiologist’s interpretation is crucial; they are trained to identify subtle signs of disease that might not be obvious to others. However, it’s important to discuss the report with your doctor, who can explain its findings in plain language and relate them to your specific symptoms and medical history. Don’t hesitate to ask questions if anything is unclear! Gut rest might be recommended as part of a treatment plan.
The Importance of a Clinical Context
An ultrasound result should never be interpreted in isolation. It’s vital that it be considered within the context of your overall clinical picture. For example, an ultrasound might show some mild thickening of the intestinal wall, but this could be due to a variety of factors—from normal anatomical variation to minor inflammation caused by dietary changes. Your doctor will take into account your symptoms, medical history, medications, and other test results to determine whether further investigation is needed.
Furthermore, it’s important to remember that ultrasound findings can sometimes be subjective – meaning different radiologists might interpret the same image slightly differently. This underscores the importance of having a qualified radiologist review your scan and provide an accurate interpretation. Ultimately, the goal isn’t just to identify abnormalities on the imaging study but to understand what those abnormalities mean in relation to your health and well-being. Autoimmune recovery can sometimes be supported by addressing gut health.
It’s also crucial to remember that this information is for general knowledge only and should not be substituted for professional medical advice. If you are experiencing digestive problems, consult with a qualified healthcare provider for an accurate diagnosis and personalized treatment plan. Allergic reactions to gut bacteria are rare but possible.