The modern world increasingly encourages stillness. We sit at desks for work, relax in front of screens during leisure time, and often rely on convenience – driving instead of walking, elevators instead of stairs. This pervasive sedentary behavior isn’t just impacting our cardiovascular health or muscle tone; it’s profoundly affecting a system many overlook until problems arise: our digestive system. For centuries, the link between physical activity and overall well-being was understood intuitively, but as lifestyles have shifted, so too has the prevalence of digestive discomfort. What was once considered an occasional issue is becoming chronic for many, and increasingly, research points to a strong correlation between prolonged inactivity and ongoing digestive trouble.
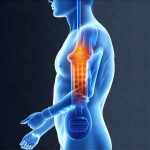
Digestive health relies on a complex interplay of factors, from the mechanical action of physical movement to the nervous system’s regulation of gut function and the microbiome’s delicate balance. A sedentary lifestyle disrupts all these elements. Reduced muscle activity slows down the entire digestive process, potentially leading to constipation, bloating, and even more serious conditions over time. Furthermore, inactivity can negatively affect the vagus nerve – a critical component in the “gut-brain axis” that governs digestion and emotional well-being. When this connection is weakened, it impacts gut motility, nutrient absorption, and overall digestive efficiency. Understanding these connections is vital for proactive health management and preventing chronic issues. If you suspect underlying issues, consider digestive problems that can be identified with testing.
The Impact of Inactivity on Digestive Processes
A fundamental aspect of healthy digestion is motility, the movement of food through the digestive tract. This isn’t solely dependent on peristalsis (the wave-like muscle contractions); it’s significantly enhanced by physical activity. When we move, gravity and muscular contractions work together to propel food downwards. A sedentary lifestyle drastically reduces these forces. Imagine a pipe with sluggish flow – things stagnate, become compacted, and potentially cause blockages or discomfort. This can manifest as:
- Constipation: Reduced motility leads to slower transit time, making stools harder and more difficult to pass.
- Bloating and Gas: Undigested food lingers longer in the colon, providing more opportunity for bacterial fermentation and gas production.
- Diverticulosis/Diverticulitis: Prolonged pressure from hardened stool can create small pouches (diverticula) in the colon wall, which can become inflamed or infected.
Beyond motility, a lack of movement impacts the digestive system’s overall efficiency. The abdominal muscles play a role in supporting internal organs and aiding in digestion. Weakened abdominal muscles contribute to poor posture, compressing the digestive tract and hindering its function. Even simple movements like walking help massage the intestines, promoting healthy bowel regularity. It’s not about intense exercise; it’s about consistent movement.
Furthermore, inactivity often leads to increased stress levels. Stress directly impacts digestion by diverting blood flow away from the gut and triggering the release of cortisol, which can disrupt digestive processes and contribute to inflammation. This creates a vicious cycle where sedentary behavior increases stress, which in turn exacerbates digestive problems. It’s essential to recognize that our bodies are designed for movement, and prolonged stillness actively undermines their natural functions. In some cases, this can be linked to issues like anemia treatments causing distress.
The Gut-Brain Axis and Sedentary Behavior
The gut and the brain are intimately connected via the gut-brain axis, a bidirectional communication network involving nerves (primarily the vagus nerve), hormones, immune pathways, and the gut microbiome. This axis influences everything from mood and cognitive function to digestion and immunity. A sedentary lifestyle can disrupt this delicate balance in several ways.
Firstly, as mentioned earlier, inactivity often weakens the vagus nerve. The vagus nerve is responsible for signaling between the brain and gut, regulating digestive processes like stomach emptying and intestinal motility. When it’s underactive, these processes become sluggish, contributing to digestive problems. Secondly, stress associated with a sedentary lifestyle (lack of social interaction, feelings of isolation) further impacts this axis. Chronic stress releases cortisol, which can alter gut permeability (“leaky gut”), allowing undigested food particles and toxins to enter the bloodstream, triggering inflammation and immune responses.
This disruption also affects the gut microbiome, the trillions of bacteria residing in our digestive tract. A healthy microbiome is crucial for digestion, nutrient absorption, and immunity. Sedentary behavior is often linked with poorer dietary choices (processed foods, high sugar intake), which negatively impact the microbiome’s composition. Inactivity can reduce microbial diversity, leading to an imbalance called dysbiosis – a state where harmful bacteria outnumber beneficial ones. Dysbiosis contributes to inflammation, impaired digestion, and increased risk of chronic diseases. A sedentary lifestyle can contribute significantly to these issues.
Inflammation and Digestive Disorders
Chronic low-grade inflammation is now recognized as a root cause of many modern health problems, including digestive disorders. A sedentary lifestyle significantly contributes to systemic inflammation through several mechanisms. Lack of physical activity reduces the body’s natural anti-inflammatory processes. Exercise releases myokines – signaling molecules that have anti-inflammatory effects and improve immune function. Without regular movement, these benefits are lost.
Moreover, inactivity promotes visceral fat accumulation – excess fat around abdominal organs. Visceral fat is metabolically active, releasing inflammatory cytokines (signaling molecules) that contribute to chronic inflammation throughout the body. This inflammation directly impacts the digestive tract, damaging the gut lining and increasing permeability. A compromised gut barrier allows harmful substances to enter the bloodstream, further fueling inflammation and creating a self-perpetuating cycle.
This chronic inflammation is implicated in various digestive disorders:
– Irritable Bowel Syndrome (IBS): Inflammation can exacerbate IBS symptoms like abdominal pain, bloating, and altered bowel habits.
– Inflammatory Bowel Disease (IBD) – Crohn’s disease and ulcerative colitis: While IBD has complex causes, inflammation plays a central role in its development and progression.
– GERD (Gastroesophageal Reflux Disease): Inflammation can weaken the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus. Sometimes GERD can cause unexpected symptoms like fatigue.
Breaking the Cycle: Integrating Movement into Daily Life
The good news is that even small changes can make a significant difference. It’s not about suddenly committing to marathon training; it’s about incorporating more movement into your everyday routine. Here are some practical steps:
- Micro-movements throughout the day: Set reminders to get up and move every 30-60 minutes. This could be as simple as walking around the office, doing a few stretches, or climbing stairs.
- Active commuting: Walk or cycle for short distances instead of driving whenever possible. Park further away from your destination.
- Incorporate movement into leisure time: Take the stairs instead of the elevator. Go for walks during lunch breaks. Engage in activities you enjoy, such as dancing, gardening, or yoga.
- Strength training: Incorporate strength training exercises to build abdominal muscles and support digestive function. Focus on core strengthening exercises.
- Mindful movement: Practices like Tai Chi and Yoga combine physical activity with mindfulness, which can help reduce stress and improve gut-brain connection.
Prioritize consistency over intensity. A 10-minute walk is more beneficial than a sporadic hour at the gym if it’s done regularly. Focus on building sustainable habits that fit your lifestyle. Remember to consult healthcare professionals for personalized guidance based on your specific health needs and any pre-existing conditions. If you experience persistent symptoms, consider whether parasites could be a factor. Ultimately, recognizing the profound connection between sedentary behavior and digestive health is the first step towards reclaiming control of your well-being and fostering a healthier, more vibrant life. Also, consider if excessive caffeine could be exacerbating issues.