The gut – often referred to as our “second brain” – is far more than just a digestive system; it’s a complex ecosystem crucial for overall health. A healthy gut facilitates nutrient absorption, supports immune function, and even influences mental wellbeing. When this intricate balance within the gut is disrupted, leading to what we broadly term ‘gut damage’, the consequences can be widespread and impact numerous aspects of life. Understanding that gut damage isn’t always about a dramatic diagnosis like Inflammatory Bowel Disease (IBD) but encompasses a spectrum of imbalances, from increased intestinal permeability (“leaky gut”) to dysbiosis (an imbalance in gut bacteria), is key to recognizing potential issues early on.
Many individuals live with subtle signs of gut dysfunction for extended periods without realizing the root cause, attributing symptoms to stress, aging, or simply “how life is.” This can delay seeking appropriate support and potentially allow minor imbalances to escalate into more chronic conditions. Identifying these warning signals isn’t about self-diagnosing; it’s about gaining awareness of your body and being proactive about your health. Recognizing the interplay between gut health and overall wellbeing empowers you to make informed decisions, explore potential causes with a healthcare professional, and implement lifestyle adjustments that support a thriving gut ecosystem. You can learn more about recognizing warning signs of gut issues.
Common Warning Signs of Gut Damage
Gut damage manifests in surprisingly diverse ways, often extending beyond digestive complaints. While bloating, gas, constipation, or diarrhea are the most obvious indicators, many symptoms can be seemingly unrelated to digestion. Chronic fatigue, despite adequate sleep, is frequently linked to an unhealthy gut as it struggles with nutrient absorption and energy production. Skin issues like eczema, psoriasis, or unexplained rashes can signal inflammation stemming from a compromised gut barrier. Even mental health concerns such as anxiety, depression, or brain fog have strong connections to the gut-brain axis – the bidirectional communication pathway between your digestive system and your brain. It’s important to remember that these symptoms aren’t necessarily caused by gut damage but can be significant indicators that warrant further investigation. Understanding signs of poor diet is also vital.
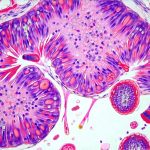
The underlying mechanisms connecting gut health to these diverse symptoms are complex. For instance, a “leaky gut” – where the intestinal lining becomes more permeable – allows undigested food particles, toxins, and bacteria to enter the bloodstream, triggering an immune response that contributes to systemic inflammation. This chronic inflammation can then exacerbate skin conditions, impact mood regulation in the brain, and deplete energy reserves leading to fatigue. Similarly, dysbiosis—an imbalance of gut bacteria—can disrupt nutrient absorption, compromise the production of vital neurotransmitters (like serotonin), and weaken the immune system’s ability to defend against pathogens. A look at imbalanced microbiome can help understand this more.
Understanding that these signs often overlap with other conditions is crucial. Don’t immediately assume a damaged gut; it’s essential to rule out other potential causes through proper medical evaluation. However, if you experience several of these symptoms concurrently or persistently, paying attention to your gut health becomes paramount. Lifestyle factors like diet, stress levels, and medication use significantly impact the gut microbiome and intestinal barrier function, making preventative measures and proactive support essential for long-term wellbeing.
Digestive Distress Signals
Digestive issues are often the most obvious sign of a problem within the gut. However, the type of digestive issue can offer clues about the nature of the imbalance. Persistent bloating, even after dietary changes, might indicate Small Intestinal Bacterial Overgrowth (SIBO) or difficulty digesting certain carbohydrates like FODMAPs. Excessive gas production could point to malabsorption issues or an overabundance of gas-producing bacteria in the gut.
Constipation isn’t just about infrequent bowel movements; it can also signify a lack of beneficial bacteria needed for proper motility and digestion. Diarrhea, conversely, might suggest inflammation, infection, or food sensitivities. Importantly, alternating between constipation and diarrhea is often a hallmark of Irritable Bowel Syndrome (IBS), which frequently stems from gut dysbiosis and increased intestinal permeability. Paying attention to the characteristics of your digestive symptoms—frequency, severity, triggers, and accompanying symptoms—can provide valuable information for identifying potential imbalances. Understanding bleeding ulcer warning signs is also important in some cases.
Beyond these common issues, other subtle signs deserve attention. Undigested food in stool indicates insufficient enzyme production or rapid transit time, potentially hindering nutrient absorption. Heartburn or acid reflux can sometimes be linked to gut dysbiosis altering stomach acidity or intestinal permeability contributing to inflammation. These digestive signals should prompt a closer look at dietary habits, stress management techniques, and potentially seeking guidance from a healthcare professional specializing in gut health.
Skin Manifestations & Inflammation
The connection between gut health and skin health is increasingly recognized. The term “gut-skin axis” describes the bidirectional relationship where imbalances in the gut microbiome can directly impact skin conditions. Chronic inflammation, often originating in the gut, plays a central role in many skin issues. Conditions like eczema (atopic dermatitis) are strongly linked to increased intestinal permeability and immune dysregulation triggered by gut imbalances. The leaky gut allows allergens and toxins to enter the bloodstream, stimulating an inflammatory response that manifests as itchy, inflamed skin.
Psoriasis, another chronic skin condition characterized by scaly patches, also has ties to gut health. Studies have shown alterations in the gut microbiome composition among individuals with psoriasis, potentially contributing to systemic inflammation. Even acne can be influenced by gut dysbiosis; imbalances may increase inflammation and hormone levels, exacerbating breakouts. Furthermore, conditions like rosacea—characterized by facial redness and flushing—have been linked to SIBO (Small Intestinal Bacterial Overgrowth).
Beyond specific skin conditions, more generalized signs of inflammation on the skin – unexplained rashes, hives, or persistent itching—can be indicators of gut dysfunction. Addressing underlying gut imbalances can often lead to significant improvements in skin health. This might involve dietary changes to reduce inflammatory foods, incorporating probiotic-rich foods or supplements to restore microbiome balance, and managing stress levels to minimize overall inflammation. It’s important to also recognize liver damage signs that can affect the skin as well.
Mental Wellbeing & Gut-Brain Connection
The gut isn’t just a digestive organ; it’s intricately connected to the brain via the gut-brain axis. This bidirectional communication pathway involves neural pathways, hormones, and immune signaling molecules that constantly exchange information between the gut and the brain. As a result, imbalances in the gut can significantly impact mood, cognitive function, and mental wellbeing.
Anxiety and depression are increasingly recognized as having strong links to gut health. The gut produces many neurotransmitters—chemical messengers crucial for regulating mood—including serotonin (often called the “happiness hormone”). Gut dysbiosis can disrupt neurotransmitter production, potentially contributing to mood disorders. Furthermore, chronic inflammation stemming from a compromised gut barrier can negatively impact brain function and increase vulnerability to anxiety and depression.
“Brain fog” – characterized by difficulty concentrating, memory problems, and mental fatigue – is another common symptom associated with gut dysfunction. Inflammatory processes in the gut can affect cognitive function and impair neuronal communication. In some cases, even neurological conditions like migraines have been linked to imbalances in the gut microbiome. Addressing gut health—through dietary changes, stress management techniques, and potentially targeted supplementation—can often lead to improvements in mental clarity, mood regulation, and overall cognitive function. The growing recognition of this connection highlights the importance of considering gut health as an integral part of holistic mental healthcare. Recognizing liver inflammation can also affect mental wellbeing.
It is crucial to consult with a qualified healthcare professional for any health concerns. This information is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.