Gastroesophageal reflux disease (GERD), commonly known as acid reflux, affects millions worldwide, causing symptoms like heartburn, regurgitation, and difficulty swallowing. For many, over-the-counter antacids or prescription medications such as proton pump inhibitors (PPIs) and H2 receptor antagonists provide significant relief. However, a substantial number of individuals experience persistent symptoms despite maximal medical therapy. This can be incredibly frustrating, impacting quality of life and leading to anxiety about potential long-term complications. Understanding why this happens and what advanced options exist beyond standard medications is crucial for those struggling with refractory reflux. It’s important to remember that navigating these complexities requires a collaborative approach between patient and healthcare provider, focused on individualized treatment plans.
The reasons behind medication resistance are multifaceted. Sometimes the diagnosis itself needs revisiting – what appears as classic GERD might actually be a different condition mimicking its symptoms (more on this later). Other times, lifestyle factors continue to exacerbate reflux even with medication, or anatomical issues prevent drugs from working optimally. Finally, some individuals develop tolerance to medications over time, requiring higher doses or alternative strategies. The goal isn’t simply escalating medication dosages indefinitely, as long-term PPI use carries its own potential risks; it’s about identifying the root cause of the persistent symptoms and addressing them proactively. This often involves a more comprehensive evaluation and exploration of options beyond traditional pharmaceutical interventions. If reflux medication stops working, it may be time to explore these options.
Advanced Diagnostic Evaluation
When initial treatments fail, a deeper dive into diagnostics is essential. Often, the standard workup – which includes symptom assessment, endoscopy (to visualize the esophagus), and potentially pH monitoring – isn’t enough to pinpoint the problem. – High-Resolution Manometry: This test measures pressure gradients within the esophagus and lower esophageal sphincter (LES). It can identify motility disorders (problems with how the esophagus contracts) or a weak LES that’s not functioning correctly, even if it appears normal on endoscopy. – Impedance-pH Monitoring: More sophisticated than traditional pH monitoring, impedance monitoring detects both acidic and non-acidic reflux episodes. This is crucial because many patients experience “silent reflux” – regurgitation without the typical heartburn sensation – which can still cause damage. These silent reflux events are often missed by standard pH testing. – Esophageal Functional Imaging (EFI): A newer technology combining manometry with impedance monitoring, EFI provides a 3D map of esophageal function, offering even more detailed insights into reflux patterns and potential contributing factors.
These advanced tests aren’t just about confirming GERD; they’re about characterizing it. Are the reflux episodes primarily acidic or non-acidic? Is there an anatomical abnormality affecting LES function? Are motility disorders playing a role? The answers to these questions guide treatment decisions, moving beyond a “one size fits all” approach. It’s also vital to rule out “GERD mimics” – conditions that present similarly but require different treatments. Examples include eosinophilic esophagitis (EoE), an allergic inflammatory condition of the esophagus; esophageal spasms; and even cardiac chest pain. Thorough evaluation can prevent misdiagnosis and ensure appropriate care. If you experience acid reflux and chest pain, seeking professional guidance is essential. Sometimes, testing used to rule out inflammation can help differentiate between conditions.
Surgical and Minimally Invasive Interventions
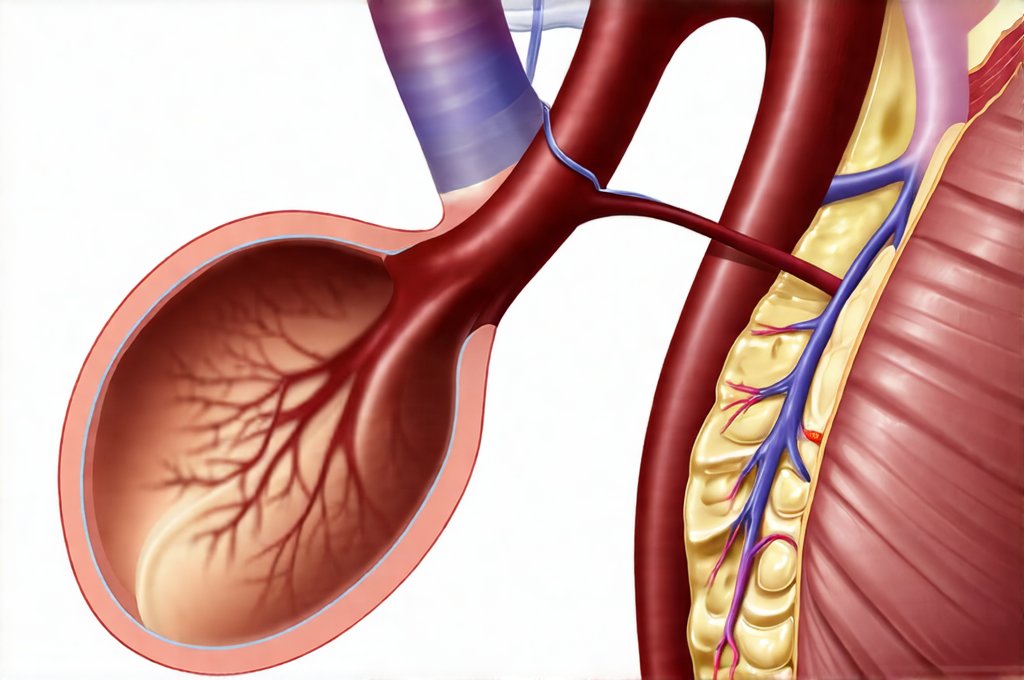
For patients with well-defined anatomical or functional issues contributing to reflux, surgical interventions may offer a long-term solution. It’s important to understand that surgery isn’t always the first line of treatment, and it’s reserved for carefully selected individuals who have failed medical management. – Fundoplication: The gold standard procedure for GERD surgery involves wrapping the upper part of the stomach (the fundus) around the lower esophagus to reinforce the LES. This creates a barrier against reflux and improves esophageal clearance. There are various types of fundoplication (Nissen, Toupet, Dor), each with its own advantages and disadvantages, determined by individual patient needs.- LINX System: A newer minimally invasive procedure involves implanting a ring of magnetic beads around the lower esophagus. These beads help to strengthen the LES without creating a permanent obstruction. – Transoral Incisionless Fundoplication (TIF): Performed through the mouth using an endoscope, TIF creates a partial fundoplication without external incisions. It’s less invasive than traditional fundoplication but may not be suitable for all patients.
These procedures are generally highly effective in reducing reflux symptoms and allowing patients to potentially reduce or eliminate medication use. However, surgery carries risks, and careful patient selection is paramount. Factors considered include the severity of reflux, presence of esophageal motility disorders, overall health, and individual preferences. Post-operative care is also critical for optimal outcomes. It’s crucial to have a detailed discussion with a surgeon experienced in GERD procedures to determine if surgery is an appropriate option. It’s also important to understand that these interventions are not cures; they aim to manage reflux by addressing its underlying causes, and lifestyle modifications remain essential even after successful surgery.
Lifestyle Modifications Revisited
While often the first recommendation, lifestyle changes frequently need re-evaluation when medication fails. It’s easy for habits to creep back in, or for patients to underestimate the impact of seemingly small choices. – Dietary Adjustments: This isn’t just about avoiding trigger foods (though identifying and eliminating those is important). It’s also about how you eat – smaller, more frequent meals; eating slowly; and avoiding lying down immediately after eating can all make a difference. Certain foods, like peppermint, chocolate, and caffeine, are known to relax the LES and should be limited.- Weight Management: Obesity significantly increases intra-abdominal pressure, forcing stomach contents upwards. Even modest weight loss can reduce reflux symptoms. – Elevating the Head of Bed: Raising the head of your bed by 6-8 inches (using blocks or a wedge pillow) helps gravity keep stomach acid where it belongs.
The key to successful lifestyle modification is consistency. It’s not about restrictive dieting or drastic changes that are unsustainable. It’s about making small, manageable adjustments that become part of your daily routine. Working with a registered dietitian can provide personalized guidance and support. Furthermore, recognizing the impact of stress on reflux is crucial. Stress often leads to poor dietary choices, increased abdominal pressure (through tension), and altered digestive function. Incorporating stress-reducing techniques like yoga, meditation, or deep breathing exercises can complement other treatment strategies.
Exploring Alternative Therapies
The landscape of GERD management extends beyond conventional medicine. While more research is needed in some areas, certain alternative therapies may offer adjunctive support for patients with refractory reflux. – Acupuncture: Some studies suggest that acupuncture may help regulate esophageal motility and reduce acid production, although the evidence remains limited.- Herbal Remedies: Certain herbs, like slippery elm and chamomile, are traditionally used to soothe the digestive tract, but caution is advised as they can interact with medications or have side effects. Always consult your doctor before using herbal remedies. – Biofeedback: This technique teaches you how to control physiological processes, such as esophageal sphincter pressure, through conscious effort.
It’s important to approach alternative therapies with a critical eye and discuss them openly with your healthcare provider. These therapies should not be seen as replacements for conventional medical treatment but rather as potential complements that may enhance overall well-being. Be wary of unsubstantiated claims or “miracle cures.” The goal is to find strategies that work for you in conjunction with evidence-based medicine, guided by a qualified healthcare professional.
Addressing the Brain-Gut Connection
Increasingly, research highlights the strong connection between the brain and gut (the “gut-brain axis”). Reflux symptoms can be significantly influenced by psychological factors like anxiety, depression, and stress. – Cognitive Behavioral Therapy (CBT): CBT helps identify and modify negative thought patterns and behaviors that contribute to reflux symptoms. It can also teach coping mechanisms for managing stress and reducing hypervigilance about bodily sensations.- Mindfulness-Based Stress Reduction (MBSR): MBSR focuses on cultivating present moment awareness and acceptance, which can reduce anxiety and improve emotional regulation, potentially lessening the impact of stress on reflux. – Visceral Hypersensitivity: Some individuals have increased sensitivity to normal digestive processes, perceiving even mild acid exposure as intense heartburn. CBT and mindfulness techniques can help modulate this hypersensitivity.
This holistic approach recognizes that GERD isn’t just a physical problem; it’s often intertwined with emotional and psychological factors. Addressing these factors can be particularly beneficial for patients who have been struggling with chronic reflux despite medical interventions. It requires acknowledging the interplay between mind and body, and integrating strategies to support both aspects of health. A collaborative approach involving gastroenterologists, therapists, and other healthcare professionals is crucial for optimizing care and improving quality of life. If acid reflux mimics heart problems are a concern, seek medical evaluation promptly. Understanding stool-based options to monitor long-term inflammation can also provide valuable insights into gut health. Consider testing used to rule out inflammation when gut pain is vague if experiencing persistent discomfort. For those struggling with symptoms, it’s helpful to know what to do when reflux symptoms appear without food intake. Finally, non-standard testing for people who don’t respond to basic treatment may uncover underlying issues.