The digestive system, often considered the unsung hero of our well-being, is far more than just a food processing plant. It’s a complex ecosystem where countless interactions occur, impacting everything from nutrient absorption to immune function and even mental health. Many individuals experience occasional digestive discomfort – bloating, gas, or changes in bowel habits – dismissing them as temporary inconveniences. However, repeated patterns of these symptoms, when investigated through thoughtful testing, can reveal valuable clues about underlying imbalances, sensitivities, or functional issues that extend beyond simple indigestion. Understanding these clues isn’t about self-diagnosing; it’s about gaining insight into your body’s unique needs and collaborating with healthcare professionals to optimize digestive health.
The challenge lies in the often subtle nature of digestive signals. Symptoms can be vague, intermittent, or mimic other conditions, making accurate assessment difficult without a systematic approach. Repeated testing isn’t necessarily about running endless tests indiscriminately; it’s about strategically choosing assessments based on initial observations and then revisiting them over time to track progress, identify triggers, and refine understanding. This iterative process allows for a more nuanced picture of what’s happening within the digestive landscape, moving beyond surface-level symptoms towards root cause identification. It acknowledges that digestion isn’t static; it’s a dynamic system influenced by diet, stress, lifestyle, and individual biochemistry. How stool testing fits into long-term digestive care can be the first step towards understanding these patterns.
Decoding Recurring Digestive Patterns
Repeated testing patterns are incredibly valuable because they move past acute events and reveal chronic trends. A single instance of bloating after eating dairy might be dismissed as a sensitivity to that particular meal. But repeated bloating consistently following dairy consumption – or even a wider range of foods – points towards something more significant, like lactose intolerance, histamine intolerance, or an underlying gut permeability issue. The same principle applies to bowel movements: occasional constipation is normal, but chronic constipation or diarrhea requires investigation. These patterns aren’t just about what symptoms are present; they’re also about when and how they occur in relation to specific factors. Consider these examples:
- Consistent bloating after consuming gluten-containing foods suggests a potential gluten sensitivity or celiac disease (requiring further testing).
- Diarrhea triggered specifically by high-FODMAP foods might indicate Irritable Bowel Syndrome (IBS) with FODMAP malabsorption as a contributing factor. Smart approaches to finding food triggers can help pinpoint these issues.
- Recurring heartburn, even with over-the-counter medication, could signal gastroesophageal reflux disease (GERD) or an issue with stomach acid production.
The key is to document these patterns meticulously – keeping a food diary, symptom journal, and noting any correlating factors like stress levels or sleep quality. This detailed record provides valuable information for healthcare providers when determining the appropriate testing strategy. It’s also important to remember that digestive symptoms often don’t exist in isolation; they can be interconnected with other seemingly unrelated health concerns, making a holistic assessment crucial. Digestive testing used in post-antibiotic care is particularly important as antibiotics disrupt the gut flora.
The Power of Functional Digestive Assessments
Traditional diagnostic tests like colonoscopies and endoscopies are essential for ruling out structural abnormalities or serious diseases. However, functional assessments delve deeper into how the digestive system is functioning – its ability to break down food, absorb nutrients, and maintain a healthy gut microbiome. Repeated functional testing can reveal subtle imbalances that wouldn’t be detected through conventional methods. One common example is a comprehensive stool analysis, which provides insights into:
- Gut microbial diversity (identifying imbalances in beneficial vs. harmful bacteria).
- Digestive enzyme levels (assessing the body’s ability to digest fats, proteins, and carbohydrates).
- Markers of inflammation (detecting signs of gut irritation or immune activation).
- Nutrient absorption rates (evaluating how well the body is utilizing vitamins and minerals).
Repeating this test after dietary changes or interventions allows for objective measurement of progress. Similarly, breath tests can assess Small Intestinal Bacterial Overgrowth (SIBO), a condition where excessive bacteria reside in the small intestine, interfering with digestion and nutrient absorption. Lactose and fructose breath tests identify carbohydrate malabsorption issues. These assessments aren’t about finding “disease”; they’re about identifying functional impairments that contribute to digestive symptoms and impacting overall health. Functional testing empowers proactive management of digestive well-being. Monitoring gut healing through follow-up testing is crucial for evaluating the effectiveness of interventions.
Identifying Food Sensitivities & Intolerances
Food sensitivities and intolerances are often at the root of chronic digestive issues, but they can be difficult to pinpoint without targeted testing. Elimination diets – removing suspected trigger foods for a period and then reintroducing them one by one while monitoring symptoms – have traditionally been the gold standard. However, food sensitivity testing (IgG/IgA antibody tests) is becoming increasingly popular. While controversial among some practitioners, repeated IgG/IgA testing can provide valuable insights when interpreted carefully alongside clinical history and symptom patterns. It’s important to understand:
- These tests don’t identify allergies (which involve IgE antibodies and are typically more immediate and severe).
- They highlight foods that the immune system is reacting to, even if symptoms aren’t dramatic.
- Repeated testing after dietary modifications can help determine whether eliminating specific foods has reduced reactivity.
It’s crucial to work with a healthcare professional experienced in interpreting these tests, as false positives are possible. Beyond antibody testing, other approaches include low-FODMAP diets (guided by a registered dietitian) and histamine intolerance protocols. The goal isn’t necessarily to eliminate foods permanently but to identify triggers and manage them effectively.
Evaluating Gut Permeability (“Leaky Gut”)
Gut permeability, often referred to as “leaky gut,” describes a condition where the intestinal lining becomes more porous, allowing undigested food particles, toxins, and bacteria to enter the bloodstream. This can trigger inflammation throughout the body and contribute to various health problems, including digestive issues, autoimmune diseases, and fatigue. While direct testing for gut permeability is still evolving, several indirect markers can suggest increased permeability:
- Zonulin levels in stool samples (zonulin is a protein that regulates intestinal permeability).
- Lactulose/mannitol breath test (measures how quickly sugars pass through the intestinal lining).
- Elevated inflammatory markers in blood tests.
Repeated testing following interventions aimed at restoring gut health – such as probiotic supplementation, dietary changes, and stress management techniques – can assess whether permeability is improving. Addressing gut permeability is often a cornerstone of long-term digestive healing. It’s essential to note that “leaky gut” isn’t a diagnosis in itself; it’s a functional impairment that requires addressing underlying causes rather than solely focusing on sealing the gut. GI testing patterns can reveal connections to immune function.
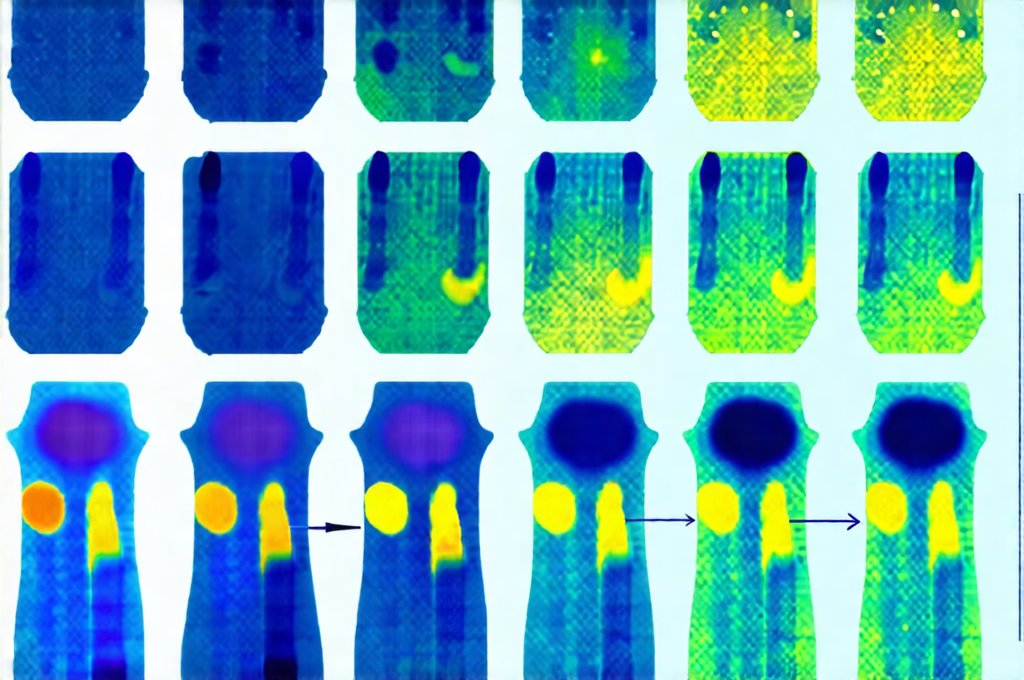
The Gut Microbiome & Repeated Assessments
The gut microbiome – the trillions of bacteria, fungi, and other microorganisms residing in our digestive tract – plays a critical role in digestion, immunity, and overall health. Dysbiosis, an imbalance in the gut microbiome, is frequently linked to digestive disorders. Comprehensive stool analysis can assess microbial diversity, identify imbalances (e.g., overgrowth of harmful bacteria), and guide probiotic selection. However, the microbiome is dynamic and influenced by numerous factors:
- Diet: Fiber intake, prebiotics, and probiotics all impact microbial composition.
- Antibiotics: Can disrupt the microbiome, leading to dysbiosis.
- Stress: Chronic stress can negatively affect gut bacteria.
Repeated stool testing after implementing dietary changes or probiotic supplementation allows for monitoring of microbial shifts and assessing whether interventions are effective. It’s important to remember that a “healthy” microbiome isn’t defined by specific bacterial species but rather by diversity and balance. The goal is to cultivate a resilient ecosystem capable of supporting optimal digestive function and overall well-being. Moreover, it’s becoming increasingly clear that the gut microbiome is highly personalized – what works for one person may not work for another, highlighting the importance of individualized approaches. Unusual testing strategies may be necessary in complex cases.