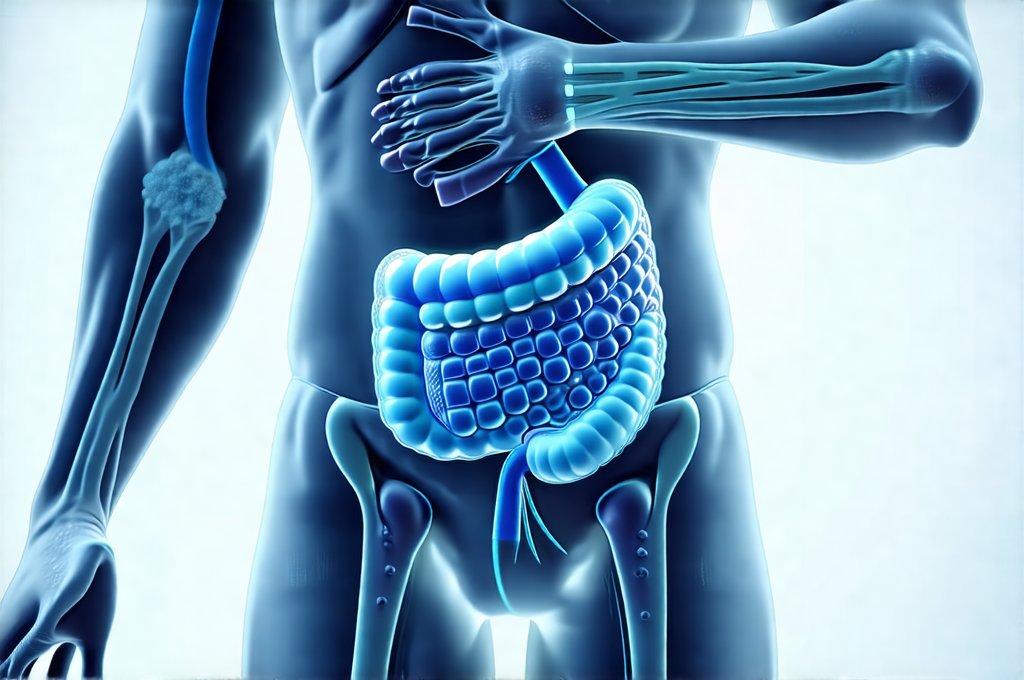
The human digestive system is an incredibly complex ecosystem, responsible for breaking down food, absorbing nutrients, and eliminating waste. For decades, we’ve understood much about its mechanical functions – peristalsis, enzymatic action, the role of different organs like the stomach and intestines. However, in recent years, a paradigm shift has occurred with the recognition that trillions of microorganisms residing within our gut play an equally, if not more significant, role in overall health. These microbial communities, collectively known as the gut microbiome, influence everything from immunity and mental wellbeing to nutrient absorption and susceptibility to chronic diseases. Traditional diagnostic methods often fall short in fully assessing the intricacies of this inner world, leading to missed diagnoses or incomplete treatment plans for digestive issues.
This is where microbiome testing emerges as a powerful tool. Unlike stool cultures which primarily identify pathogenic (disease-causing) bacteria, microbiome tests analyze the composition and diversity of the entire microbial community – identifying both beneficial and potentially harmful species. They can reveal imbalances known as dysbiosis, assess functional capacity (what the microbes are actually doing), and provide insights into specific metabolic pathways impacting digestion and overall health. While not a replacement for conventional diagnostics, microbiome testing offers an unprecedented level of detail that complements traditional approaches and empowers more personalized interventions. It’s important to note that this technology is still evolving, but its potential to revolutionize how we understand and address digestive issues is undeniable. You may also want to explore digestive exams as another diagnostic tool.
Dysbiosis & Common Digestive Complaints
Dysbiosis, simply put, refers to an imbalance in the gut microbiome – a disruption of the delicate ecosystem where beneficial bacteria are outnumbered by potentially harmful ones or overall diversity is reduced. This isn’t necessarily about the presence of “bad” bacteria; it’s often about the absence of enough “good” bacteria to keep things in check. Several common digestive complaints can be strongly linked to specific patterns of dysbiosis identified through microbiome testing. For example, individuals experiencing chronic bloating or gas may exhibit a reduction in methane-utilizing bacteria, leading to increased hydrogen production and fermentation within the gut. Similarly, those with Irritable Bowel Syndrome (IBS) often show reduced microbial diversity and alterations in key bacterial groups involved in short-chain fatty acid (SCFA) production – SCFAs being crucial for gut health and inflammation regulation.
Microbiome testing can pinpoint these imbalances, allowing healthcare practitioners to tailor interventions accordingly. It’s important to remember that dysbiosis is rarely a standalone issue; it’s often intertwined with lifestyle factors like diet, stress, antibiotic use, and environmental exposures. A test result revealing low levels of Akkermansia muciniphila, for instance – a bacterium known for strengthening the gut barrier – might prompt dietary changes to increase prebiotic fiber intake or explore probiotic supplementation focused on supporting this species. This is a far more targeted approach than simply recommending a generic probiotic. Consider also exploring food energy patterns for dietary insights.
The power lies in moving beyond symptom management and addressing the root cause, which often resides within the microbial landscape of the gut. Furthermore, testing can help differentiate between various subtypes of IBS based on microbiome profiles, guiding treatment strategies to address specific mechanisms driving symptoms. It’s crucial however, that these tests are interpreted by qualified healthcare professionals who understand the nuances of microbiome data and can integrate it with other clinical information. If you need further digestive diagnostics before surgery, look into digestive tests.
Small Intestinal Bacterial Overgrowth (SIBO) & Microbiome Insights
Small Intestinal Bacterial Overgrowth (SIBO) is a condition where an excessive amount of bacteria resides in the small intestine – an area that normally contains relatively few microbes. Traditionally diagnosed using breath tests measuring hydrogen and methane gas production after consuming specific sugars, microbiome testing offers complementary information about SIBO, particularly regarding the types of bacteria involved. While a breath test indicates the presence of excess bacteria, it doesn’t identify which species are contributing to the overgrowth.
Microbiome analysis can reveal whether the overgrowth is dominated by typically colonic (large intestine) bacteria migrating upwards, or by opportunistic species already present in the small intestine. This distinction is important because it impacts treatment strategies. For instance, an overgrowth predominantly composed of colonic bacteria might suggest underlying motility issues contributing to bacterial translocation. – Identifying specific bacterial populations can also help predict treatment response to different antimicrobial therapies used for SIBO. – Furthermore, microbiome testing can assess the impact of SIBO on overall gut health and identify potential nutrient deficiencies resulting from bacterial competition or altered absorption. It’s helpful to understand signs that your gut might be struggling too.
It’s important to note that a positive breath test doesn’t always equate to symptomatic SIBO, and vice versa. Microbiome data provides an additional layer of information to refine diagnosis and personalize treatment plans, often in conjunction with traditional testing methods. A comprehensive approach considers both the quantity and quality of bacteria present within the small intestine.
Inflammatory Bowel Disease (IBD) & Microbial Signatures
Inflammatory Bowel Disease (IBD), encompassing conditions like Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the digestive tract. While the exact causes remain complex, microbiome dysbiosis plays a significant role in both the development and progression of IBD. Microbiome testing can help identify specific microbial signatures associated with different subtypes of IBD and predict disease flares. For example, reduced microbial diversity, decreased abundance of Faecalibacterium prausnitzii (a key anti-inflammatory bacterium), and increased levels of pro-inflammatory bacteria have been consistently observed in IBD patients.
Importantly, microbiome analysis can also reveal the extent of gut barrier dysfunction – a hallmark of IBD – by assessing markers like zonulin and calprotectin which are linked to microbial activity. This information is vital for tailoring dietary interventions aimed at reducing inflammation and restoring gut integrity. – Microbiome tests can also assess the impact of different medications used in IBD treatment on the microbial community, helping optimize therapeutic strategies. Home kits are available to help detect digestive infections too.
However, it’s crucial to understand that microbiome profiles associated with IBD are highly variable between individuals. Testing isn’t a diagnostic tool for IBD itself (diagnosis requires endoscopy and biopsy), but rather provides valuable insights into the underlying mechanisms driving disease activity and can inform personalized management strategies alongside conventional treatments. It helps move beyond a “one-size-fits-all” approach to IBD care.
Leaky Gut & Microbiome Markers
“Leaky gut,” more formally known as increased intestinal permeability, refers to a compromised barrier function in the intestines allowing undigested food particles, toxins, and bacteria to escape into the bloodstream. While not universally recognized as a distinct medical condition, increased intestinal permeability is often implicated in various health issues including autoimmune diseases, allergies, and chronic inflammation. Microbiome testing can offer indirect evidence of leaky gut by assessing several key markers.
One approach involves analyzing levels of zonulin – a protein released in response to microbial imbalances that contributes to loosening the tight junctions between intestinal cells. Elevated zonulin levels suggest increased permeability. Furthermore, microbiome tests can identify bacterial species known to either strengthen or compromise the gut barrier. For instance, Akkermansia muciniphila strengthens the mucus layer protecting the gut lining, while certain pro-inflammatory bacteria can contribute to barrier disruption. – Analyzing short-chain fatty acid (SCFA) production is also informative, as SCFAs like butyrate nourish intestinal cells and enhance barrier function.
Reduced SCFA levels or altered SCFA profiles can indicate a compromised gut barrier. It’s important to note that assessing leaky gut through microbiome testing is indirect; other tests like lactulose/mannitol breath test are more directly indicative of permeability. However, microbiome data provides valuable context and helps identify potential microbial drivers contributing to increased intestinal permeability, guiding interventions aimed at restoring gut health and strengthening the barrier function. You might also consider seasonal recipes that align with your digestive needs.
It’s essential to remember that microbiome testing is a relatively new field, and ongoing research continues to refine our understanding of its applications and limitations. While it offers promising insights into digestive issues and beyond, it should always be interpreted within a broader clinical context by qualified healthcare professionals. It’s not about seeking a “cure” based on test results but rather using the information to personalize interventions that support overall gut health and wellbeing. You can also explore one-skillet meals for digestive ease.