The gut—often called our “second brain”—plays an incredibly vital role in overall health, extending far beyond just digestion. It’s a complex ecosystem where trillions of microorganisms interact with our immune system, influence mental wellbeing, and even impact chronic disease risk. When illness strikes – whether it’s a viral infection, bacterial overgrowth, or prolonged stress – the delicate balance within this ecosystem can be disrupted, leading to gut dysbiosis and potential damage to the intestinal lining. This damage isn’t always obvious; symptoms can range from bloating and fatigue to more systemic issues like autoimmune flares and mood disturbances. Therefore, assessing the extent of gut repair after illness is crucial for targeted interventions and a successful recovery journey.
Traditionally, gut health assessments were limited, relying heavily on subjective symptom reporting. However, advancements in testing technologies now offer a much deeper understanding of what’s happening within our digestive system. These tests can provide valuable insights into inflammation levels, microbial diversity, intestinal permeability (often referred to as “leaky gut”), and nutrient absorption capabilities. Importantly, it’s essential to remember that these tests aren’t diagnostic tools in the traditional sense; they are informational resources best interpreted by a qualified healthcare practitioner who understands your individual health context. Choosing the right test(s) depends on the specific illness experienced, symptoms present, and overall health goals, making personalized assessment key. For athletes or highly active people, gut tests can be particularly insightful.
Understanding Gut Permeability & Testing Options
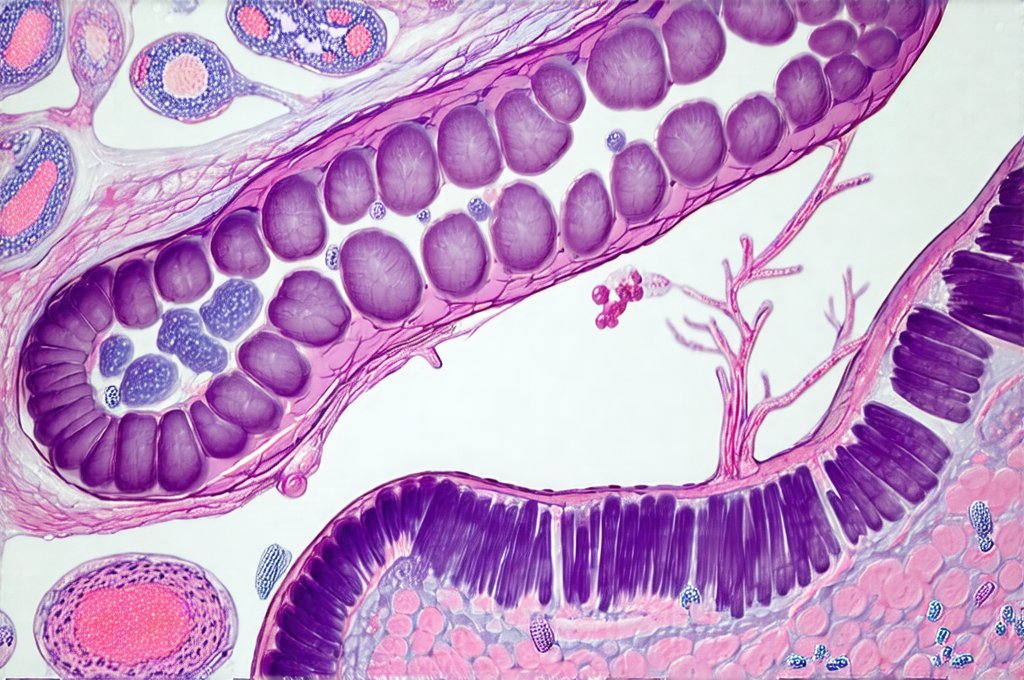
Gut permeability refers to how tightly or loosely the cells lining our intestinal wall are connected. A healthy gut has a tight barrier, allowing nutrients to be absorbed while keeping harmful substances like undigested food particles, toxins, and bacteria contained within the digestive tract. When this barrier weakens – becoming more permeable – these unwanted elements can “leak” into the bloodstream, triggering an immune response and contributing to systemic inflammation. This is where the term “leaky gut” originates, although it’s increasingly recognized as a functional impairment rather than a disease itself. Testing for gut permeability aims to assess the presence of larger protein molecules in the stool, indicating that the intestinal barrier isn’t functioning optimally.
Several tests attempt to evaluate gut permeability. One common method is the lactulose-mannitol test, which involves consuming these two sugar molecules and then measuring their levels in urine. Lactulose is a large molecule that should remain mostly undigested if the gut lining is intact, while mannitol (a smaller molecule) is readily absorbed. An elevated lactulose level combined with normal mannitol levels suggests increased intestinal permeability. However, this test can be affected by factors like transit time and digestive enzyme activity, so it’s not always perfectly accurate. Another emerging approach involves measuring zonulin in stool – zonulin is a protein that regulates tight junctions between intestinal cells; elevated levels may indicate a compromised barrier function. It’s important to note that these tests are still evolving and should be used as part of a comprehensive assessment, rather than relied upon solely for diagnosis. Often after travel or illness, gentle gut healing is the best approach.
Beyond direct permeability testing, markers of inflammation can also suggest gut barrier dysfunction. Elevated calprotectin in stool, for example, indicates intestinal inflammation which often accompanies increased permeability. The key takeaway is that assessing gut permeability isn’t always straightforward, and combining different tests with clinical evaluation provides the most accurate picture.
Identifying Microbial Imbalances: Stool Testing
Stool testing has become increasingly sophisticated, moving beyond simple culture-based methods to utilize DNA sequencing technologies. These advanced tests – often called microbiome analysis – can identify the diverse range of microorganisms residing in your gut, including bacteria, fungi, viruses and archaea. They provide a detailed breakdown of microbial composition, highlighting both beneficial and potentially harmful species. A healthy gut microbiome is characterized by diversity—a wide array of different organisms working synergistically. Conversely, dysbiosis involves reduced diversity and an overgrowth of opportunistic pathogens.
- Stool tests can identify specific deficiencies in keystone bacteria crucial for digestion, immune function, and nutrient synthesis.
- They may also reveal the presence of harmful bacteria associated with inflammation or digestive issues like Clostridium difficile.
- Importantly, microbiome analysis provides a baseline to track changes over time as you implement dietary or lifestyle interventions aimed at gut repair.
However, it’s crucial to understand that interpreting stool tests requires expertise. The microbiome is incredibly complex and varies significantly between individuals based on factors such as diet, genetics, and environment. Simply identifying imbalances isn’t enough; a skilled practitioner can help determine the underlying causes and develop targeted strategies for restoring microbial balance, which might include dietary changes, probiotics, prebiotics, or lifestyle modifications. It’s also vital to choose reputable testing labs that employ rigorous quality control measures and provide clear, actionable reports. Top fermented foods can help support a healthy microbiome.
Assessing Digestive Function: Comprehensive Stool Analysis & Beyond
While microbiome analysis focuses on who is living in your gut, comprehensive stool analysis (CSA) delves deeper into what the gut is actually doing. CSAs evaluate various markers of digestive function, including levels of pancreatic enzymes, bile acids, short-chain fatty acids (SCFAs), and inflammatory markers like calprotectin. Pancreatic enzyme insufficiency can lead to maldigestion and nutrient deficiencies, while imbalances in bile acid metabolism may contribute to bloating or diarrhea. SCFAs, produced by beneficial bacteria during fiber fermentation, are essential for gut health and overall wellbeing; low levels suggest insufficient fiber intake or microbial dysbiosis.
- CSAs also assess markers of fat absorption, providing insights into potential issues with lipid digestion.
- They can identify signs of parasitic infections which may contribute to digestive symptoms and inflammation.
- This detailed information allows for a more targeted approach to gut repair, addressing specific deficiencies or imbalances in digestive capacity.
Beyond CSAs, other tests can assess specific aspects of digestive function. Breath tests, for example, can detect the presence of small intestinal bacterial overgrowth (SIBO), where excessive bacteria proliferate in the small intestine leading to fermentation and gas production. Hydrogen and methane levels are measured after consuming a sugar solution; elevated levels suggest SIBO. Similarly, food intolerance testing – while controversial – may help identify foods that trigger digestive symptoms or inflammation. Again, these tests should be interpreted by a qualified healthcare professional who can integrate them into the broader clinical picture. After overeating, meal ideas can aid in recovery.
Nutrient Status & Gut Repair: Blood Testing Considerations
Gut health directly impacts nutrient absorption. When the intestinal lining is compromised, it can lead to deficiencies in essential vitamins and minerals. Therefore, assessing nutrient status through blood testing is an integral part of tracking gut repair after illness. Specifically, consider evaluating levels of vitamin D, B12, iron, zinc, and magnesium – all crucial for immune function, energy production, and overall wellbeing. Deficiencies in these nutrients can further weaken the gut barrier and hinder recovery.
- Blood tests should also evaluate markers of inflammation such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
- Assessing albumin levels provides insight into protein absorption capacity which is often impaired in a damaged gut.
- Furthermore, testing for amino acid imbalances can reveal deficiencies in building blocks essential for tissue repair and immune function.
It’s important to note that standard nutrient panels may not always accurately reflect intracellular nutrient levels – the amount of nutrients actually available within cells. More advanced tests like intracellular nutrient analysis can provide a more accurate assessment, but they are often more expensive and require specialized interpretation. Ultimately, blood testing serves as a valuable tool for identifying nutrient deficiencies and guiding supplementation strategies to support gut repair and restore optimal health. If you suspect skin issues related to your gut, GI tests can be helpful. It’s also important to know how to support healing.
The information provided in this article is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment. Also consider if grains are necessary.