Chronic inflammation is often called “silent suffering” for good reason. It underlies many prevalent health concerns—from autoimmune diseases and digestive issues to skin conditions and even mood disorders. While we frequently associate inflammation with acute injuries like sprains, the persistent, low-grade inflammation that characterizes much modern illness can be remarkably difficult to pinpoint. Increasingly, research points to food as a significant driver of this chronic inflammation for many individuals. Identifying these food triggers isn’t always straightforward; what causes inflammation in one person might be perfectly benign for another. This is where diagnostics come into play, offering tools to help unravel the complex relationship between diet and inflammatory responses within the body.
Traditionally, diagnosing food-related inflammation relied heavily on elimination diets – a process that can be lengthy, frustrating, and prone to subjective interpretation. Modern diagnostic testing provides more objective insights, moving beyond guesswork and towards targeted dietary modifications. These tests aren’t about identifying allergies (which involve an IgE immune response with rapid onset symptoms); they aim to uncover food sensitivities or intolerances, which elicit a delayed inflammatory response mediated by the IgG pathway, often manifesting as subtle but pervasive symptoms. It’s crucial to understand that these are distinct processes, and diagnostic approaches differ accordingly. This article will explore various diagnostics available to reveal food-triggered inflammation, their strengths, limitations, and how they fit into a holistic approach to health.
Food Sensitivity & Intolerance Testing
Food sensitivity and intolerance tests have evolved significantly in recent years. Early generations were often criticized for lacking scientific rigor and producing unreliable results. However, newer methodologies, coupled with increased understanding of the immune system, are leading to more dependable assessments. The most common type is IgG food sensitivity testing. These tests measure levels of IgG antibodies against various foods in a blood sample. Elevated IgG levels suggest that your body has repeatedly encountered a particular food protein, potentially triggering an inflammatory response over time. It’s important to remember: IgG positivity doesn’t necessarily mean you have to avoid the food entirely. It simply indicates potential reactivity and warrants further investigation.
These tests typically assess a broad panel of foods – often exceeding 90 common items – including dairy, gluten, eggs, soy, corn, nuts, and fruits. Results are usually presented as tiered levels of IgG reactivity (low, moderate, high), offering guidance on which foods to potentially eliminate or reduce in the diet. While convenient, IgG testing isn’t without its critics. Some argue that IgG antibodies represent tolerance rather than reactivity; however, growing evidence suggests they can correlate with symptom flares in sensitive individuals. A key factor is interpreting results within the context of a patient’s overall health picture and symptoms – it should never be used as a standalone diagnostic tool.
Beyond IgG testing, other methods are emerging. Component-Resolved Diagnostics (CRD) offer more granular analysis by identifying specific protein components within foods that trigger reactivity. This is particularly useful for individuals with suspected allergies or sensitivities to common allergens like milk or wheat, allowing for a more precise understanding of which proteins are problematic. Another approach involves assessing markers of intestinal permeability (“leaky gut”), as increased permeability can contribute to food sensitivity development and systemic inflammation. These tests often measure zonulin levels in stool samples.
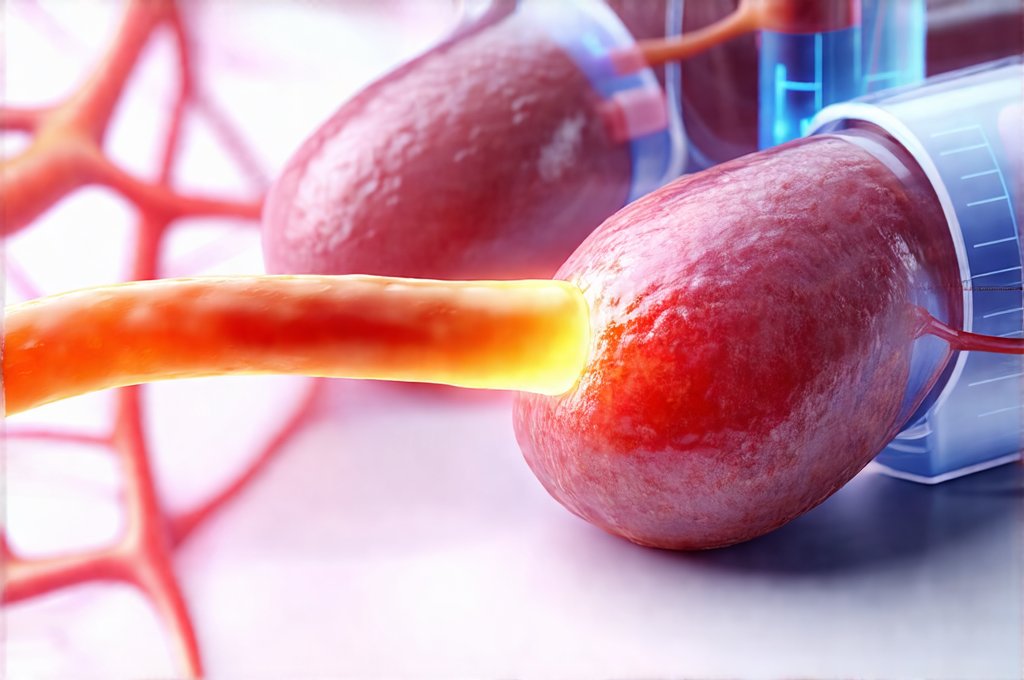
Inflammatory Markers & Blood Analysis
While food sensitivity testing identifies potential triggers, measuring inflammatory markers directly provides a broader picture of the body’s overall inflammatory state. Several blood tests are commonly used to assess inflammation, offering valuable insights when combined with dietary investigations. C-reactive protein (CRP) is an acute phase reactant produced by the liver in response to inflammation. Elevated CRP levels indicate systemic inflammation but don’t pinpoint its source; it could be due to infection, injury, or food sensitivities. However, tracking CRP changes alongside dietary modifications can help assess whether removing specific foods reduces overall inflammation.
Another key marker is erythrocyte sedimentation rate (ESR), which measures how quickly red blood cells settle at the bottom of a test tube. Faster settling rates suggest inflammation, but like CRP, it’s non-specific. More sophisticated tests include measuring cytokines – small proteins involved in immune signaling. Cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) are elevated during inflammatory responses. Assessing these markers can provide a more nuanced understanding of the specific immune pathways activated by food sensitivities. Furthermore, assessing levels of secretory IgA (sIgA) in stool samples can offer insight into gut health; low sIgA suggests impaired intestinal immunity and increased susceptibility to inflammation.
It’s important to note that inflammatory marker results should be interpreted cautiously, considering factors like age, stress levels, and underlying medical conditions. A single elevated marker isn’t necessarily cause for alarm but rather a signal to investigate further. Combining these blood analyses with food sensitivity testing provides the most comprehensive assessment. This allows healthcare professionals to correlate specific foods with changes in inflammatory markers, leading to more targeted dietary interventions. When symptoms persist, consider hidden signs that might indicate further testing is needed. For those experiencing digestive discomfort after stressful events, diagnostics can help pinpoint the cause.
Stool Analysis & Gut Microbiome Testing
The gut microbiome—the trillions of bacteria residing in our digestive tract—plays a crucial role in both immune function and inflammation. An imbalance in the gut microbiome (dysbiosis) can contribute to increased intestinal permeability, allowing undigested food particles to enter the bloodstream and trigger an inflammatory response. Stool analysis provides valuable information about the composition and diversity of your gut microbiome. Tests can identify imbalances in bacterial populations, as well as potential pathogens or markers of inflammation within the gut.
Comprehensive stool testing often includes assessments for: – Calprotectin (a marker of intestinal inflammation) – Zonulin (as mentioned previously, indicating intestinal permeability) – Short-chain fatty acids (SCFAs), which are produced by beneficial bacteria and have anti-inflammatory properties – Levels of various bacterial species, identifying imbalances. Analyzing these parameters can help identify whether gut dysbiosis is contributing to food-triggered inflammation. It’s also important to understand that dietary changes themselves significantly impact the microbiome; therefore, stool testing should be repeated after implementing dietary modifications to assess their effectiveness.
Furthermore, some advanced tests evaluate digestive capacity – assessing pancreatic enzyme function and bile acid metabolism. Impaired digestion can lead to incomplete breakdown of food proteins, increasing their likelihood of triggering an immune response. The gut is often the epicenter of food-related inflammation, making stool analysis a critical component of any comprehensive diagnostic approach. This testing helps move beyond simply identifying what foods are problematic and delves into why your body might be reacting to them in the first place—addressing the root cause rather than just managing symptoms. If you suspect medication side effects, GI checkups can provide valuable insight. Understanding blood markers is also key to evaluating overall inflammation levels. Don’t underestimate the value of low-cost diagnostics, which can provide a starting point for investigation.
It’s essential to emphasize that these diagnostics, while valuable, aren’t definitive solutions. They are tools to guide personalized dietary interventions under the guidance of a qualified healthcare professional – ideally one experienced in functional medicine or integrative nutrition. Self-diagnosing and drastically restricting your diet based solely on test results can be counterproductive and potentially lead to nutritional deficiencies. A collaborative approach that combines diagnostic testing with careful symptom tracking, dietary modifications, and ongoing monitoring offers the best path towards identifying and managing food-triggered inflammation. Gut diagnostics can further clarify the link between stress and digestion.