Digestive symptoms are incredibly common, ranging from occasional discomfort to debilitating chronic conditions. Many times, these symptoms are transient and resolve on their own with simple lifestyle adjustments. However, recognizing when digestive distress is escalating beyond a typical upset requires careful attention and can be crucial for seeking appropriate care. Ignoring persistent or worsening symptoms can lead to delayed diagnosis of underlying issues, potentially impacting long-term health. This article will explore key checkpoints to watch during the progression of digestive symptoms, empowering you with knowledge to better understand your body and advocate for your well-being. It’s important to remember that this information is not a substitute for professional medical advice; it’s intended to provide a framework for understanding when further investigation might be necessary.
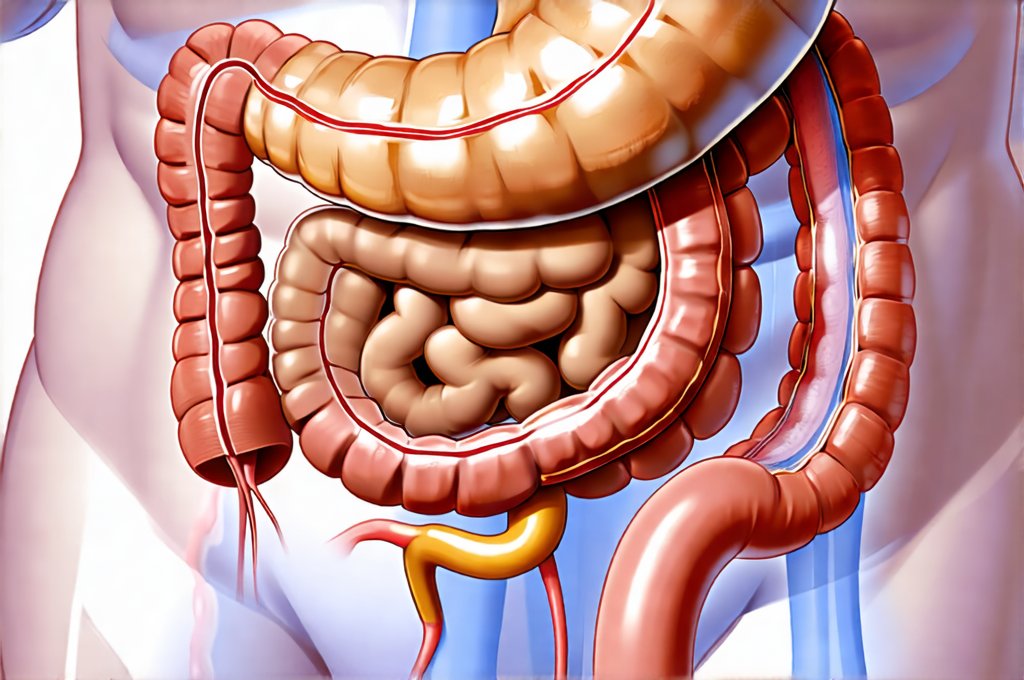
The gut is an incredibly complex system, intimately linked to overall health and wellbeing. From nutrient absorption to immune function, its role is far-reaching. Consequently, digestive symptoms are rarely isolated events. They can be indicators of underlying dietary sensitivities, stress responses, or even more serious medical conditions. Being attuned to the nuances of your digestive experience – what feels different, when changes occur, and how they impact your daily life – allows you to identify potentially concerning patterns early on. Paying attention isn’t about inducing anxiety; it’s about being proactive in protecting your health. A mindful approach to recognizing symptom progression is a powerful tool for navigating the complexities of digestive health. Considering comfort-based food routines can also contribute to better gut health.
Recognizing Escalating Symptoms: Red Flags & Patterns
Often, digestive symptoms start subtly. Perhaps a little bloating after certain foods or occasional heartburn. These are generally manageable and don’t necessarily warrant immediate medical attention. However, patterns and escalating intensity are what signal potential problems. A key checkpoint is the frequency of your symptoms. Is it happening more often? Are episodes becoming longer in duration? For instance, if occasional bloating transitions into near-constant discomfort that interferes with daily activities, it’s time to take notice. Another important factor is the severity of your discomfort – is it moving beyond mild annoyance to significant pain or distress?
Beyond frequency and intensity, pay attention to new symptoms emerging alongside existing ones. If heartburn is suddenly accompanied by difficulty swallowing (dysphagia), that’s a different story than just occasional acid reflux. Similarly, if diarrhea starts occurring with abdominal pain and fever, it suggests something more than a simple stomach bug. These additions aren’t merely “added discomfort”; they can indicate the development of a new or worsening condition. Finally, watch for changes in your bowel habits – alterations in stool consistency (hard, soft, watery), frequency, color, or the presence of blood are all significant indicators that warrant medical evaluation. Simple ways to upgrade your routine can help manage these symptoms.
Understanding these patterns requires self-awareness and honest assessment. It’s easy to dismiss symptoms as “just stress” or “something I ate,” but consistently ignoring changes can delay diagnosis. Keeping a symptom journal – recording what you eat, when your symptoms occur, their severity, and any accompanying factors – can be incredibly helpful in identifying these patterns and presenting a clear picture to your healthcare provider. This isn’t about self-diagnosing; it’s about being informed and prepared for a productive conversation with medical professionals. Digestive support foods kept on hand can also ease discomfort.
When To Seek Immediate Medical Attention: Emergency Symptoms
While many digestive symptoms develop gradually, some require immediate medical attention. These aren’t situations where you can “wait and see.” Severe abdominal pain, particularly if it’s sudden, intense, and doesn’t improve with over-the-counter remedies, is a major red flag. This could indicate conditions like appendicitis, bowel obstruction, or ectopic pregnancy (in women). Similarly, vomiting blood – even small amounts – requires urgent medical evaluation. The color of vomit can also be telling; coffee ground-like emesis suggests digested blood and necessitates immediate attention.
Another critical symptom is rectal bleeding, especially if it’s significant or accompanied by dizziness, weakness, or fatigue. While minor rectal bleeding can sometimes occur from hemorrhoids, persistent or substantial bleeding warrants a prompt medical assessment to rule out more serious conditions like colorectal cancer or inflammatory bowel disease. Finally, difficulty breathing, severe dehydration (indicated by decreased urination, extreme thirst, and dizziness), or signs of shock (rapid heartbeat, confusion) alongside digestive symptoms are all indicators of a life-threatening situation that requires immediate emergency care.
It’s crucial to trust your instincts in these situations. Don’t hesitate to seek medical attention if you feel something is seriously wrong. Delaying treatment can have severe consequences. Knowing the difference between manageable discomfort and potentially dangerous symptoms is vital for protecting your health. Remember, erring on the side of caution is always preferable when it comes to serious medical concerns. Planning ahead with travel periods can minimize distress.
Navigating Chronic Digestive Issues: Long-Term Concerns
Chronic digestive issues – such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) like Crohn’s disease and ulcerative colitis, or celiac disease – often present a more complex diagnostic challenge. These conditions typically don’t come on suddenly; they develop over time with fluctuating symptoms. A key checkpoint here is the persistence of symptoms despite lifestyle modifications and over-the-counter treatments. If dietary changes, stress management techniques, and basic remedies aren’t providing relief after several weeks, it’s time to seek medical evaluation.
Another concern is unintended weight loss. Significant or unexplained weight loss alongside chronic digestive symptoms can indicate malabsorption issues, inflammation, or even cancer. It’s important to differentiate between intentional weight loss through diet and exercise versus a decline in weight that you haven’t actively pursued. Similarly, fatigue that doesn’t improve with rest – especially if it accompanies other digestive symptoms – could be a sign of underlying inflammation or nutritional deficiencies. This is particularly true if the fatigue significantly impacts your daily functioning.
Finally, look for signs of systemic involvement. Chronic digestive diseases can sometimes affect other parts of the body. For example, joint pain, skin rashes, eye inflammation, or mouth sores alongside digestive symptoms might suggest an autoimmune component like IBD. These extra-intestinal manifestations are crucial clues that help doctors arrive at an accurate diagnosis and develop a comprehensive treatment plan. Early diagnosis and management of chronic conditions are essential for minimizing long-term complications and improving quality of life. Comfort meals can provide some relief during these times.
The Role of Dietary Changes & Food Sensitivities
Diet plays a massive role in digestive health, and changes in your diet can often exacerbate or alleviate symptoms. A significant checkpoint is identifying potential food sensitivities or intolerances. This isn’t necessarily the same as a food allergy (which involves an immune response); it’s more about how your body reacts to certain foods. If you consistently experience bloating, gas, diarrhea, or constipation after consuming specific foods – even if they’re generally considered healthy – it warrants investigation.
- Consider keeping a detailed food diary alongside your symptom journal.
- Try an elimination diet under the guidance of a healthcare professional. This involves removing potential trigger foods for a period and then reintroducing them one at a time to observe any reactions.
- Pay attention to common culprits like gluten, dairy, lactose, fructose, or artificial sweeteners.
It’s important not to self-diagnose food sensitivities without proper testing. Sometimes, what appears to be a food sensitivity is actually an underlying digestive issue that needs to be addressed. However, making mindful dietary changes – such as increasing fiber intake, staying hydrated, and reducing processed foods – can often significantly improve digestive health. If you suspect a specific food intolerance, consult with a registered dietitian or your doctor before making drastic changes to your diet. Understanding menstrual bloating phases is also key for some individuals.
Stress & The Gut-Brain Connection: A Crucial Link
The gut and brain are intimately connected through what is known as the gut-brain axis. Stress can significantly impact digestive function, and conversely, digestive issues can contribute to stress and anxiety. A key checkpoint here is recognizing how your stress levels correlate with your digestive symptoms. Do you notice that your bloating or diarrhea worsens during periods of high stress? Are you experiencing increased digestive discomfort when feeling anxious or overwhelmed?
Stress can disrupt the normal motility of the gut, leading to constipation, diarrhea, or IBS flare-ups. It can also increase inflammation and alter the composition of your gut microbiome – the community of bacteria that live in your digestive tract. Managing stress through techniques like mindfulness meditation, yoga, deep breathing exercises, or regular physical activity can often help alleviate digestive symptoms.
If you’re struggling to manage stress on your own, consider seeking support from a therapist or counselor. Addressing underlying emotional factors is crucial for improving both mental and digestive health. Remember that prioritizing self-care and incorporating stress-reducing practices into your daily routine are essential components of overall well-being and can have a profound impact on your digestive system. Smart eating habits during stressful times, like the holidays, can also make a difference.