The intricate relationship between our mental state and digestive function is far more profound than many realize. For centuries, we’ve understood intuitively that “nervous stomachs” exist—that anxiety can directly impact how we process food. However, recent advances in gut diagnostics are revealing exactly how stress wreaks havoc on digestion at a physiological level, explaining the connection beyond mere anecdotal experience. It’s not simply about feeling unwell; it’s about demonstrable changes to gut motility, microbiome composition, and even intestinal permeability. Understanding these mechanisms is key to proactively supporting digestive health in the face of modern stressors.
This isn’t just about occasional anxiety before a big event. Chronic stress – the persistent low-grade worry that characterizes much of modern life – is particularly damaging. It continuously activates the body’s stress response, leading to a cascade of hormonal and neurological effects that persistently disrupt digestive processes. This article will explore the diagnostic tools now available to understand these disruptions and how they illuminate the pathways through which stress impacts gut health, moving beyond symptoms towards root causes. We’ll examine what tests can reveal about your individual digestive function when under stress, and how this knowledge empowers a more targeted approach to wellness. Considering stress recovery strategies is often the first step towards improved gut health.
The Gut-Brain Axis: A Two-Way Street
The concept of the gut-brain axis isn’t new, but its complexity is continually being uncovered. It refers to the bidirectional communication network between the gastrointestinal tract and the brain. This connection isn’t just neurological; it involves hormonal signals, immune pathways, and – crucially – the microbiome. Stress triggers a series of events that disrupt this carefully balanced system. When we perceive a threat (physical or emotional), the hypothalamic-pituitary-adrenal (HPA) axis is activated, leading to the release of cortisol—the “stress hormone.” While cortisol is essential for survival in acute situations, chronically elevated levels have detrimental effects on digestion.
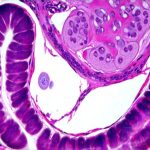
Cortisol impacts gut motility – the movement of food through the digestive tract. It can either speed things up, causing diarrhea, or slow them down, leading to constipation. Furthermore, it alters intestinal permeability (“leaky gut”), making the gut lining more porous and allowing undigested food particles and toxins to enter the bloodstream, potentially triggering inflammation. The microbiome also suffers; stress reduces microbial diversity, favoring less beneficial bacteria and increasing populations of those associated with dysbiosis – an imbalance in gut flora. This isn’t a one-way street either: the gut microbiome itself influences brain function, affecting mood, cognition, and even stress response. Understanding gut sensitivity is paramount when addressing these issues.
This interconnectedness is why stress can manifest so differently for different people; some experience bloating and abdominal pain, while others struggle with changes in appetite or develop irritable bowel syndrome (IBS)-like symptoms. Understanding this axis is crucial to understanding the diagnostic approaches needed to assess the impact of stress on individual digestive health. The goal isn’t just symptom management, but addressing the underlying imbalances that have arisen due to chronic activation of the stress response and its consequences for gut function. A good starting point can be exploring weekend recovery meals to help reset digestion.
Diagnostic Tools for Uncovering Gut Dysfunction
Traditional digestive testing often focuses on identifying specific pathogens or deficiencies. However, when it comes to stress-induced digestive issues, a more comprehensive approach is necessary—one that assesses multiple aspects of gut health simultaneously. Several advanced diagnostic tools are becoming increasingly available:
- Comprehensive Stool Analysis: This remains a cornerstone assessment. Beyond identifying parasites and bacteria (beneficial & harmful), modern stool tests now analyze markers like calprotectin (an indicator of inflammation) and secretory IgA (reflecting immune function). They also provide detailed microbiome analysis, quantifying different bacterial species and assessing overall diversity. Looking at short-chain fatty acid (SCFA) production can reveal how well your gut bacteria are fermenting fiber – a crucial aspect of gut health often compromised by stress.
- Breath Testing: Small intestinal bacterial overgrowth (SIBO) is common in individuals experiencing chronic stress, as altered motility allows bacteria to migrate from the colon into the small intestine. Breath tests measure hydrogen and methane levels after consuming specific sugars, indicating bacterial fermentation and potential SIBO.
- Food Sensitivity & Intolerance Testing: While not directly related to stress causing sensitivities, stress can exacerbate existing intolerances or even contribute to the development of new ones by increasing intestinal permeability. Identifying trigger foods is essential for managing symptoms.
- Organic Acids Testing (OAT): This assesses metabolic markers in urine, providing insights into gut microbiome function, nutrient absorption, and detoxification pathways – all areas impacted by stress and dysbiosis.
Deep Dive: Microbiome Sequencing
Microbiome sequencing has revolutionized our understanding of the gut’s microbial ecosystem. It goes far beyond simply identifying which bacteria are present; it quantifies their abundance and provides insights into their functional capabilities. This is particularly relevant in the context of stress, as we know stress drastically alters microbiome composition.
– A healthy microbiome is characterized by high diversity – a wide range of different bacterial species. Stress tends to reduce this diversity, making the gut more vulnerable to imbalances.
– Specific bacteria are associated with resilience and stress buffering; for example, Faecalibacterium prausnitzii produces butyrate, an anti-inflammatory short-chain fatty acid that protects the gut lining. Assessing these key species can help determine how effectively your microbiome is supporting digestive health.
– The functional potential of the microbiome—what metabolic processes it’s capable of – is also important. Stress can reduce the production of beneficial metabolites like SCFAs, compromising nutrient absorption and immune function. Implementing kitchen rhythms can help support a healthy microbiome.
Analyzing microbiome sequencing data requires expertise; interpreting the results isn’t as simple as identifying “good” and “bad” bacteria. Context matters. Factors such as diet, medication use, and lifestyle all influence the microbiome, so a holistic approach is essential for accurate interpretation and personalized recommendations.
Understanding Intestinal Permeability (“Leaky Gut”)
As mentioned earlier, chronic stress increases intestinal permeability – often referred to as “leaky gut.” This means the tight junctions between cells in the intestinal lining become more porous, allowing larger molecules (undigested food particles, toxins, bacteria) to enter the bloodstream. This triggers an immune response, leading to inflammation and potentially contributing to systemic health problems.
– Zonulin is a protein that regulates intestinal permeability. Stress can increase zonulin levels, loosening those tight junctions. While direct testing for zonulin in stool or blood exists, it’s still debated how reliably these tests reflect the overall state of gut barrier function.
– Lactulose/Mannitol Breath Test (LMB): This is currently considered a more reliable non-invasive method to assess intestinal permeability. It involves consuming lactulose and mannitol sugars, then measuring their levels in breath over several hours. Lactulose is a larger molecule that should be poorly absorbed in a healthy gut; increased lactulose absorption suggests a leaky gut.
– Addressing leaky gut requires a multi-faceted approach: reducing stress, supporting the microbiome with probiotics and prebiotics, incorporating anti-inflammatory foods into your diet, and potentially using targeted supplements to support gut barrier function (under professional guidance). It’s important to consider strategic meal layers as well.
Assessing Gut Motility & Digestive Enzyme Production
Beyond microbiome imbalances and increased permeability, stress disrupts the physical processes of digestion. Altered gut motility – how quickly food moves through the digestive tract – is a common consequence.
– Gastric Emptying Studies: These can assess how long it takes for food to leave the stomach. Delayed gastric emptying (slow digestion) can contribute to bloating, fullness, and nausea, while rapid emptying can lead to diarrhea.
– SIBO breath testing indirectly assesses motility, as altered motility is a key factor in its development.
– Digestive enzyme production can also be affected by stress. Insufficient enzymes mean food isn’t broken down efficiently, leading to malabsorption and digestive discomfort. While direct enzyme function tests aren’t readily available, OATs can provide clues about nutrient deficiencies that might suggest inadequate digestion or absorption.
– Supporting gut motility involves strategies like regular exercise, adequate hydration, fiber intake, and stress management techniques. Addressing enzyme deficiency may involve incorporating fermented foods (containing natural enzymes) or considering targeted enzyme supplementation (again, under professional guidance). Understanding hydration-timed meals can also be beneficial.
The key takeaway is this: digestive health isn’t just about what you eat; it’s about how your body processes food, and that process is profoundly influenced by your mental state. The advanced diagnostics discussed here provide a window into these complex interactions, empowering individuals to take a proactive approach to gut health and resilience in the face of stress.