Gastrointestinal (GI) distress is an incredibly common experience, impacting millions globally. Symptoms like bloating, abdominal pain, changes in bowel habits, nausea, and heartburn can be disruptive and concerning, often leading individuals to fear the worst – a serious underlying GI condition. While many of these symptoms are caused by relatively benign issues such as dietary sensitivities or temporary infections, it’s vital to differentiate them from more severe possibilities like inflammatory bowel disease (IBD), celiac disease, or even gastrointestinal cancers. Navigating this process can be stressful, and understanding the diagnostic tools available – both lab tests and imaging scans – is a crucial step in achieving peace of mind and appropriate care. This article will explore some of these key investigations used to help rule out serious GI issues, focusing on what they assess and how results are interpreted, always emphasizing the importance of professional medical evaluation.
The initial assessment typically begins with a detailed patient history and physical examination conducted by a healthcare provider. These foundational steps guide the selection of appropriate diagnostic testing, preventing unnecessary procedures while ensuring no potential concerns are overlooked. It’s important to remember that no single test definitively “rules out” all GI conditions; rather, a combination of tests, coupled with clinical judgment, is used to build a comprehensive picture and arrive at an accurate diagnosis. This process often involves a tiered approach, starting with less invasive options and progressing to more complex investigations if needed. The goal isn’t simply to identify disease but also to understand the cause of symptoms, allowing for targeted treatment strategies and improved patient outcomes. Consider incorporating supportive food rituals into your routine as a proactive step.
Laboratory Investigations: Uncovering Clues in Blood and Stool
Laboratory tests are frequently the first line of defense when investigating GI issues. They provide objective data that can help pinpoint areas of concern and guide further investigations. Blood tests, in particular, offer a wealth of information about overall health and specific markers related to digestive function and inflammation. Common blood tests include a complete blood count (CBC) which assesses for signs of infection or anemia; electrolytes to evaluate hydration and balance; liver function tests to assess the health of the liver, which plays a role in digestion; and inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which can indicate inflammation within the GI tract.
Stool tests are equally valuable. They can identify infections caused by bacteria, viruses, or parasites, detect evidence of bleeding (occult blood), and assess for malabsorption issues. A particularly important stool test is the fecal calprotectin test, which measures a protein released by white blood cells during inflammation in the intestines – a strong indicator of IBD or other inflammatory conditions. Additionally, tests can be performed to look for Clostridium difficile (C. diff) toxin, especially after antibiotic use, as C. diff infection is a common cause of diarrhea and colitis. It’s essential to understand that abnormal lab results don’t automatically equal a serious diagnosis; they merely flag areas requiring further evaluation. Supporting your gut with portable snacks can help manage symptoms in between testing.
The interpretation of laboratory findings requires expertise. For example, elevated CRP levels can be caused by numerous factors beyond GI inflammation, such as infections or autoimmune diseases. Similarly, positive stool tests for bacteria may not always signify infection; some bacteria are part of the normal gut flora. Therefore, these results must be considered within the context of the patient’s symptoms, medical history, and other diagnostic findings. A healthcare professional will integrate all available data to arrive at a reasoned conclusion and determine the next steps in the evaluation process. Understanding how sleep and digestion are connected can also provide valuable insight.
Imaging Scans: Visualizing the GI Tract
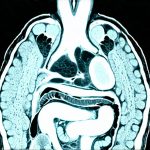
When lab tests suggest or fail to fully explain GI symptoms, imaging scans become invaluable tools for visualization. These scans allow doctors to directly observe the structure and function of the digestive system, identifying abnormalities that might not be detectable through other means. There are several types of imaging modalities commonly used in GI diagnostics, each with its strengths and weaknesses. X-rays, while less frequently used as a primary diagnostic tool now, can still be helpful for identifying blockages or perforations. Computed tomography (CT) scans provide more detailed cross-sectional images and are particularly useful for detecting tumors, abscesses, and inflammation throughout the abdomen.
Magnetic resonance imaging (MRI) offers even greater detail than CT scans, especially for soft tissues, making it ideal for evaluating the bowel wall and surrounding structures. However, MRI can be more time-consuming and expensive than CT scanning. Endoscopy, involving a flexible tube with a camera inserted into the digestive tract, provides direct visualization of the esophagus, stomach, or colon. During endoscopy, biopsies can be taken to examine tissue samples under a microscope for signs of inflammation, infection, or cancer. Capsule endoscopy involves swallowing a small capsule containing a camera that transmits images as it travels through the small intestine – an area difficult to visualize with traditional endoscopic methods. Focusing on thermal recipes can provide comfort and aid digestion during this process.
The choice of imaging modality depends on the suspected diagnosis and the specific region of the GI tract being investigated. For instance, if colon cancer is suspected, a colonoscopy is typically performed; if abdominal pain suggests appendicitis, a CT scan may be ordered. It’s important to note that imaging scans are not without risks, such as exposure to radiation from CT scans or potential complications associated with endoscopy. Therefore, the benefits of each scan must be carefully weighed against its potential drawbacks before proceeding.
Understanding Specific Scan Results and Their Implications
The interpretation of imaging results requires specialized knowledge. For example, a CT scan revealing “thickening” of the bowel wall is often suggestive of inflammation characteristic of IBD or Crohn’s disease. However, thickening can also occur due to other conditions like diverticulitis or even benign polyps. Therefore, further evaluation, such as endoscopy with biopsy, is usually necessary to confirm the diagnosis. Similarly, an MRI showing “hyperintensity” on certain sequences may indicate edema (swelling) in the bowel wall, suggesting active inflammation.
Colonoscopy results are often described based on polyp findings – size, location, and type. Adenomatous polyps, which have the potential to become cancerous, require removal and follow-up monitoring. Capsule endoscopy can reveal subtle bleeding sources or signs of malabsorption that might be missed with other methods. It’s crucial to remember that a “normal” scan doesn’t necessarily rule out all GI issues; some conditions may not be visible on imaging scans, especially in the early stages. The results must always be interpreted in conjunction with clinical findings and laboratory data. Incorporating herb-infused foods may offer gentle support during this time.
Finally, it is vital for patients to openly discuss scan results with their healthcare provider. Asking questions about the implications of the findings, potential next steps, and any concerns they may have is crucial for informed decision-making and effective management of their health. The diagnostic process can be complex, but a collaborative approach between patient and doctor ensures the best possible outcome. Implementing gut reset relief strategies may also prove beneficial.
It’s also important to remember that anxiety surrounding GI symptoms is common, and seeking reassurance from medical professionals is a healthy step towards managing those fears. Understanding the available diagnostic tools and how they are used can empower patients to actively participate in their own care and navigate the evaluation process with greater confidence. Food rituals can also play a role in calming anxiety around digestion.