The sudden, urgent need to rush to the bathroom isn’t always just about something you ate. While dietary indiscretions certainly play a role, frequent or unexpected urges to defecate can signal a more complex interplay of physiological factors, psychological states, and even underlying medical conditions. Most people experience occasional bowel urgency – that feeling of needing to go right now – without issue. However, when this becomes a regular occurrence, interfering with daily life or accompanied by other symptoms, it’s important to understand the potential reasons beyond simple digestive upset. Ignoring persistent urgency isn’t just uncomfortable; it could be overlooking a signal from your body that needs attention.
This article delves into some of the less obvious causes behind urgent bowel movements, moving past common explanations like food intolerance and focusing on the subtle connections between mind and gut, hormonal influences, neurological factors, and potential medical conditions warranting further investigation. It’s crucial to remember this is for informational purposes only and should not replace professional medical advice. If you are experiencing concerning symptoms, consulting a healthcare provider is always the best course of action. Understanding these possibilities can empower you to advocate for your health and engage in more informed conversations with your doctor.
The Mind-Gut Connection & Bowel Urgency
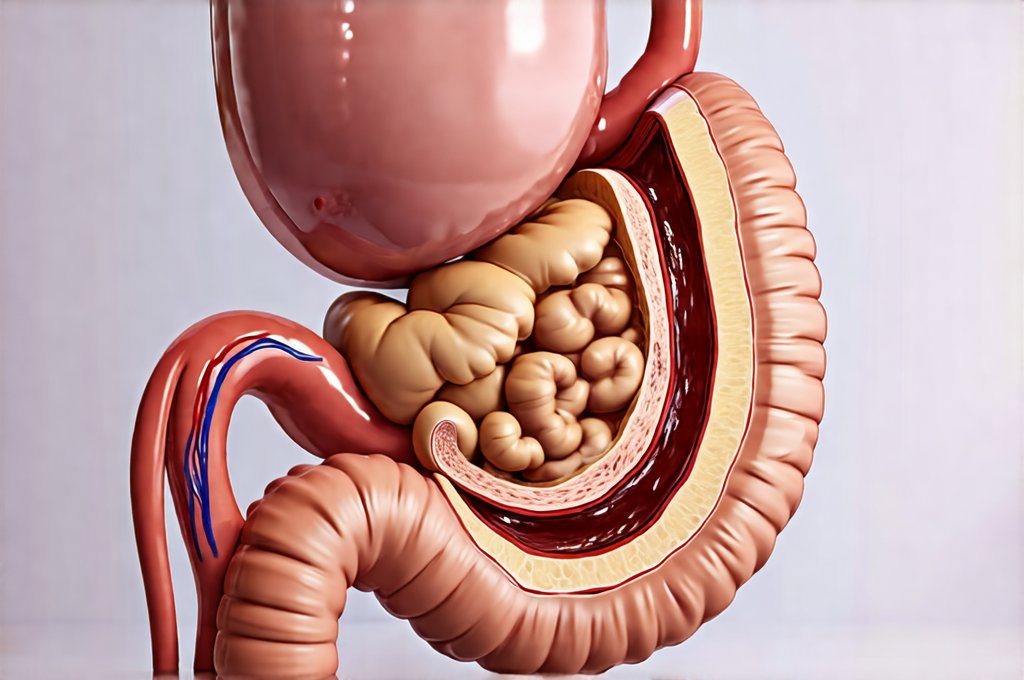
The intricate relationship between our brains and digestive systems – often referred to as the gut-brain axis – is becoming increasingly recognized as a significant factor in bowel function. It’s not simply a one-way street; signals travel constantly both ways. Stress, anxiety, and even seemingly minor emotional fluctuations can have a profound impact on intestinal motility (the movement of food through your digestive tract), potentially leading to urgency. This is because the brain influences gut activity via the autonomic nervous system, which controls involuntary functions like digestion.
- During times of stress, the sympathetic nervous system (“fight or flight”) kicks in, often accelerating bowel movements.
- Conversely, chronic stress can disrupt normal gut function, contributing to conditions like Irritable Bowel Syndrome (IBS) where urgency is a hallmark symptom.
- Psychological factors like fear or anticipation (even thinking about needing to use the bathroom!) can trigger muscle contractions in the rectum, creating an immediate urge.
This explains why some individuals experience increased bowel urgency during periods of high stress – before a big presentation, during travel, or even when facing everyday anxieties. The gut isn’t just responding to physical stimuli; it’s highly attuned to our emotional state. Furthermore, conditions like panic disorder can manifest with pronounced gastrointestinal symptoms, including sudden and overwhelming urges to defecate. Addressing underlying mental health concerns may therefore be a crucial step in managing bowel urgency for some individuals. Understanding digestive enzymes can also help support the digestive process.
Hormonal Influences & the Digestive System
Hormones play an essential role in regulating numerous bodily functions, including digestion. Fluctuations in hormone levels – particularly in women – can significantly impact bowel habits and contribute to feelings of urgency. This is largely due to the influence of estrogen and progesterone on gut motility and sensitivity. During different phases of the menstrual cycle, pregnancy, or menopause, these hormonal shifts can lead to noticeable changes in digestive function.
For example, elevated levels of progesterone during certain phases of the menstrual cycle tend to slow down intestinal motility, potentially leading to constipation. However, as hormone levels shift again, this can be followed by increased urgency and diarrhea. Similarly, pregnancy causes substantial hormonal changes that affect the entire digestive system, often resulting in altered bowel habits throughout gestation. Menopause is another period where fluctuating hormones can contribute to digestive disturbances, including urgent bowel movements. Beyond sex hormones, thyroid disorders can also disrupt digestive function; both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) are associated with changes in bowel motility, potentially causing urgency or constipation.
It’s important to note that the connection between hormonal fluctuations and bowel urgency is complex and individual experiences vary greatly. If you suspect a hormonal imbalance might be contributing to your symptoms, discussing this with your healthcare provider is essential for proper diagnosis and management. It may also be helpful to test for triggers that exacerbate these issues.
Identifying Potential Underlying Medical Conditions
While psychological factors and hormones often play a role, persistent or severe bowel urgency can sometimes signal an underlying medical condition that requires attention. It’s vital to differentiate between functional issues (like IBS) and structural problems within the digestive system.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis cause chronic inflammation of the digestive tract, often leading to frequent diarrhea, abdominal pain, and urgency.
- Microscopic Colitis: This condition involves inflammation in the colon that can only be detected through microscopic examination of a biopsy. It commonly presents with watery diarrhea and urgent bowel movements.
- Celiac Disease: An autoimmune reaction to gluten, celiac disease damages the small intestine, leading to malabsorption and digestive symptoms including urgency, bloating, and diarrhea.
Recognizing these possibilities doesn’t mean self-diagnosing; it means being proactive about seeking medical evaluation if your symptoms are persistent or concerning. Your doctor may recommend tests such as stool analysis, blood work, colonoscopy, or endoscopy to help determine the underlying cause of your bowel urgency. Understanding alternative therapies can also be a component of management for some conditions.
Dietary Factors Beyond Intolerance
While food intolerances (like lactose intolerance) are well-known triggers for digestive upset and urgency, there are other dietary factors that can contribute to these symptoms. FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols) are short-chain carbohydrates that are poorly absorbed in the small intestine. When they reach the large intestine, they’re fermented by bacteria, producing gas and potentially leading to bloating, cramping, and urgency.
- A low-FODMAP diet, often recommended for people with IBS, can help identify if these carbohydrates are contributing to your symptoms.
- Excessive caffeine consumption can stimulate bowel movements and increase urgency in some individuals.
- Artificial sweeteners (sorbitol, mannitol) found in sugar-free products can also have a laxative effect.
Furthermore, rapid dietary changes – such as suddenly increasing fiber intake without adequate hydration – can temporarily disrupt digestive function and cause urgency. Maintaining a balanced diet with sufficient fiber and fluids is crucial for optimal bowel health. It’s about finding what works best for your individual system through mindful observation and potentially working with a registered dietitian. Being aware of hidden ingredients in food can also make a difference.
When to Seek Medical Attention
It’s normal to experience occasional episodes of bowel urgency, particularly after eating something that doesn’t agree with you. However, there are certain warning signs that warrant prompt medical attention. Do not delay seeking professional help if:
- You experience sudden and severe changes in your bowel habits.
- Your bowel urgency is accompanied by rectal bleeding, abdominal pain, fever, or weight loss.
- You notice blood in your stool.
- You have a family history of colon cancer or IBD.
- Bowel urgency significantly interferes with your daily life and quality of life.
These symptoms could indicate a more serious underlying condition that requires diagnosis and treatment. Remember, early detection is often key to successful management of digestive disorders. Your healthcare provider can help determine the cause of your bowel urgency and recommend appropriate interventions, whether it’s dietary modifications, medication, or further testing. The goal isn’t just to manage the symptoms; it’s to understand the root cause and address it effectively for long-term health and well-being. A high-fat diet can also contribute to bowel issues, so understanding its effect is important. Also, knowing how to read labels helps in avoiding problematic foods. Finally, understanding the hormone-bowel link is key to a holistic approach.