Long COVID, also known as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), presents a bewildering array of symptoms that can persist for months – even years – after the initial acute phase of illness. Unlike many infections where recovery marks a return to baseline, Long COVID often involves new or exacerbated health problems impacting multiple organ systems. While the exact mechanisms driving these prolonged effects remain under intense investigation, increasing evidence points toward significant disruptions in the gut microbiome and its interplay with the immune system as key contributors to symptom development and persistence. This isn’t necessarily about direct viral presence within the gut long after acute infection; it’s more about how the initial infection, and the body’s response to it, fundamentally alters the ecosystem within our digestive tract.
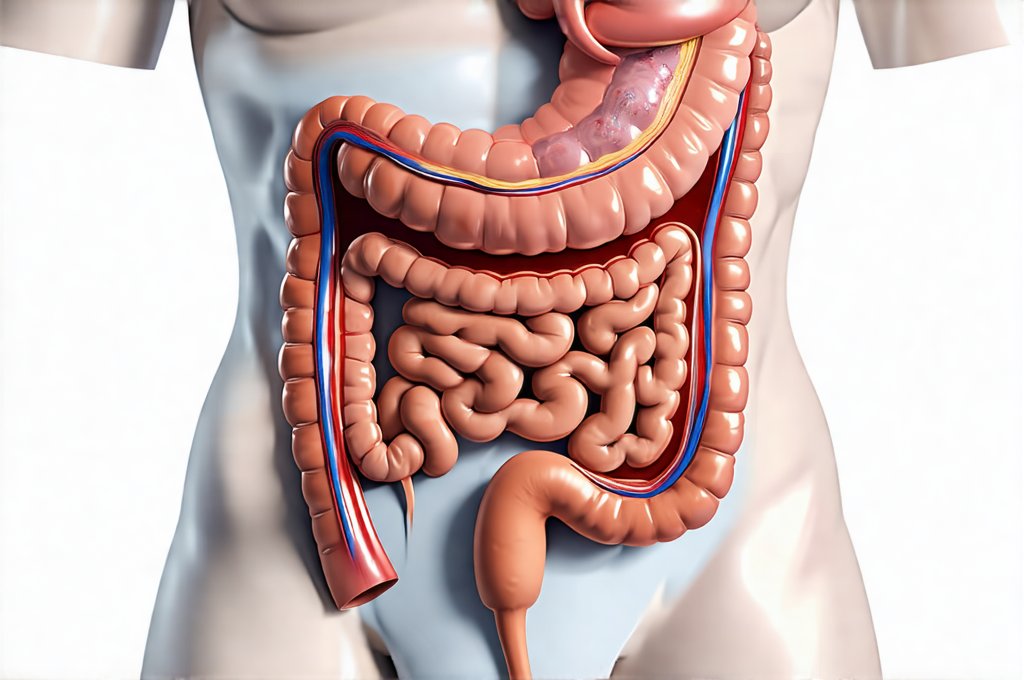
The gut microbiome—the vast community of bacteria, viruses, fungi, and other microorganisms residing in our intestines—plays a crucial role in maintaining overall health. It influences everything from digestion and nutrient absorption to immune function, mental wellbeing, and even hormone regulation. SARS-CoV-2 infection can profoundly disrupt this delicate balance, leading to dysbiosis – an imbalance in the gut microbial composition. This dysbiosis is thought to contribute significantly to Long COVID symptoms through several interconnected pathways including increased intestinal permeability (“leaky gut”), immune dysregulation, altered metabolite production, and potentially even neuroinflammation. Understanding how these changes occur and identifying specific patterns of gut microbiome disruption are now central goals for researchers seeking more effective diagnostics and therapies for Long COVID sufferers. Considering strategic meal layers can also aid in managing these disruptions.
Gut Testing Methodologies in Long COVID Research
The growing recognition of the gut’s role in Long COVID has spurred a surge in research utilizing various gut testing methodologies to characterize microbial imbalances and identify potential therapeutic targets. These tests aren’t simply about identifying which bacteria are present; they aim to understand how these microbes interact with each other and the host, and how those interactions influence disease processes. Currently, the most commonly employed techniques fall into several categories, each with its own strengths and limitations.
- 16S rRNA gene sequencing: This is arguably the most prevalent method used in gut microbiome research due to its relative affordability and ease of implementation. It focuses on a specific gene sequence (the 16S rRNA gene) found in bacterial DNA, allowing researchers to identify different bacterial taxa present in a sample. However, it doesn’t provide information about the functionality of those bacteria or their metabolic activity – just their identity.
- Whole Genome Sequencing (WGS): WGS provides a much more detailed picture of the microbial community by sequencing the entire genome of all organisms present in a sample. This allows for identification of not only bacterial species but also strains, genes involved in metabolism, and potential virulence factors. It is significantly more expensive than 16S rRNA gene sequencing and requires substantial computational resources for data analysis.
- Metabolomics: Unlike methods that directly assess microbial composition, metabolomics examines the metabolic products of gut microbes – the small molecules they produce during digestion and other processes. This provides a functional readout of what’s happening in the gut and can reveal alterations in key metabolic pathways associated with Long COVID symptoms.
- Fecal Microbiota Transplantation (FMT) analysis: While FMT itself is a treatment, analyzing donor and recipient microbiome profiles before and after transplantation helps understand how specific microbial communities influence symptom relief or persistence.
These techniques are often used in combination to gain a more comprehensive understanding of the gut microbiome’s role in Long COVID. For example, 16S sequencing might identify dysbiosis while metabolomics reveals functional changes associated with it, and WGS can pinpoint specific genes driving those alterations. This multi-faceted approach is crucial for developing targeted interventions that address the root causes of gut-related symptoms in Long COVID. A gut reset diet could be a starting point to rebalance the microbiome.
The Gut-Immune Axis & Long COVID Symptoms
The connection between the gut microbiome and the immune system—often referred to as the gut-immune axis—is central to understanding many aspects of Long COVID. A healthy gut microbiome helps “train” the immune system, promoting tolerance to harmless antigens while maintaining the ability to effectively respond to pathogens. Disruption of this balance can lead to chronic inflammation and autoimmune responses that contribute significantly to a wide range of symptoms experienced by individuals with Long COVID.
One key mechanism linking gut dysbiosis and Long COVID is increased intestinal permeability, often called “leaky gut.” When the barrier function of the intestinal lining is compromised, bacterial components (like lipopolysaccharide or LPS) can leak into the bloodstream, triggering systemic inflammation. This chronic low-grade inflammation has been implicated in symptoms like fatigue, brain fog, muscle aches, and even cardiovascular complications seen in Long COVID patients. Furthermore, SARS-CoV-2 infection itself can directly damage the intestinal barrier, exacerbating this issue. Stress from dealing with a long term illness can also contribute; high stress jobs are known to trigger gut symptoms.
The gut microbiome also influences immune cell populations, including T cells and B cells. Dysbiosis can lead to imbalances in these cells, resulting in impaired antibody production, reduced T cell function, and potentially contributing to autoimmune phenomena. Emerging research suggests that certain microbial metabolites—short-chain fatty acids (SCFAs) produced by gut bacteria—play a critical role in modulating immune responses and reducing inflammation. Reduced SCFA production due to dysbiosis could further compromise immune regulation in Long COVID patients.
Exploring Specific Gut Markers & Symptom Correlations
Researchers are actively identifying specific gut microbial markers that correlate with different Long COVID symptoms, offering potential diagnostic and therapeutic targets. For instance:
- Reduced Akkermansia muciniphila: This bacterium is known to strengthen the intestinal barrier and promote immune homeostasis. Studies have shown lower levels of Akkermansia in Long COVID patients, particularly those with gastrointestinal symptoms. Supplementation with Akkermansia or strategies to increase its abundance through dietary changes are being investigated as potential interventions.
- Increased Pathobionts: Certain bacteria, known as pathobionts, can become opportunistic pathogens when the gut ecosystem is disrupted. Elevated levels of these microbes in Long COVID patients have been linked to increased inflammation and symptom severity. Common examples include Klebsiella pneumoniae and certain strains of Escherichia coli.
- Altered SCFA Production: As mentioned previously, SCFAs are crucial for immune regulation and gut health. Dysbiosis can reduce the production of beneficial SCFAs like butyrate, propionate, and acetate, contributing to inflammation and impaired gut barrier function.
Analyzing these markers through gut testing can help personalize treatment strategies by identifying specific microbial imbalances that need to be addressed. It’s important to note, however, that correlation doesn’t equal causation – more research is needed to determine whether these microbial changes are a cause or consequence of Long COVID symptoms. Understanding gut pH shifts can also help in understanding symptom persistence.
The Role of Metabolomics in Uncovering Functional Changes
Metabolomics offers a powerful complement to microbiome sequencing by providing insights into the functional consequences of gut dysbiosis. Rather than simply identifying which bacteria are present, metabolomic analysis reveals what those bacteria are actually doing—the metabolic products they’re producing and how these metabolites impact host physiology.
- Tryptophan Metabolism: Alterations in tryptophan metabolism have been consistently observed in Long COVID patients. Tryptophan is an essential amino acid that plays a vital role in immune function and neurotransmitter production. Gut bacteria play a key role in metabolizing tryptophan into various compounds, some of which are beneficial (e.g., serotonin) while others can be detrimental. Dysbiosis can disrupt this process, leading to imbalances in tryptophan metabolites associated with inflammation and neurological symptoms.
- Bile Acid Metabolism: The gut microbiome also influences bile acid metabolism – a process critical for fat digestion and absorption. Altered bile acid profiles have been observed in Long COVID patients, potentially contributing to gastrointestinal symptoms and metabolic dysfunction.
- SCFA Imbalance: Metabolomic analysis can quantify specific SCFA levels, providing a more detailed understanding of gut microbial activity and its impact on inflammation and immune regulation.
Limitations & Future Directions for Gut Testing in Long COVID
Despite the growing promise of gut testing in Long COVID research, several limitations must be acknowledged. Firstly, the gut microbiome is incredibly complex and varies significantly between individuals based on factors like diet, genetics, lifestyle, and geographic location. This makes it challenging to establish “normal” microbial profiles and identify consistent biomarkers for Long COVID. Secondly, many studies rely on fecal samples, which may not accurately reflect the entire microbial composition of the digestive tract. Emerging technologies like capsule endoscopy and intestinal biopsies offer more comprehensive sampling methods but are invasive and expensive.
Future research should focus on:
- Longitudinal Studies: Tracking changes in the gut microbiome over time in Long COVID patients to understand how it evolves with disease progression and treatment response.
- Larger, Well-Characterized Cohorts: Recruiting larger study groups with detailed clinical data to improve statistical power and identify robust biomarkers.
- Integration of Multi-Omics Data: Combining microbiome sequencing, metabolomics, proteomics, and other “omics” approaches to gain a more holistic understanding of the gut’s role in Long COVID.
- Development of Personalized Interventions: Using gut testing results to tailor dietary recommendations, probiotic formulations, or other therapies to address individual microbial imbalances.
Ultimately, unlocking the secrets of the gut microbiome is crucial for developing effective diagnostics and treatments for this complex and debilitating condition. Understanding gut biofeedback can also play a role in management. And finally, consider how high-satiety meals may influence the gut microbiome and overall health during recovery.