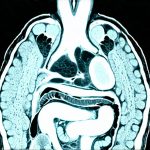
The human gut – often referred to as our ‘second brain’ – is an astonishingly complex ecosystem. It’s far more than just a digestive tract; it’s intricately linked to everything from our immune system and mental wellbeing to nutrient absorption and even chronic disease risk. For years, diagnosing issues within the gut relied heavily on subjective symptoms, invasive procedures like colonoscopies, or broad-stroke testing that often missed subtle but significant problems. Increasingly, however, advanced imaging techniques, particularly “gut scans,” are offering a more precise and non-invasive way to assess gut health, helping clinicians rule out serious organ complications with greater accuracy. These scans aren’t simply about finding tumors; they’re about understanding the functional state of the digestive system – how it’s moving food, absorbing nutrients, and interacting with its vast microbial community. Understanding how to maintain gut health while eating out can also contribute to a proactive approach.
The evolution of gut scan technology represents a paradigm shift in gastroenterological diagnostics. Traditional methods often struggled to pinpoint the root cause of chronic abdominal pain, bloating, or changes in bowel habits. Patients might undergo multiple tests, leaving them frustrated and without a definitive diagnosis. Gut scans provide a detailed visualization of the digestive tract, revealing abnormalities that were previously difficult or impossible to detect. This allows for earlier intervention, more targeted treatment plans, and ultimately, improved patient outcomes. It’s important to remember that gut scans aren’t meant to replace traditional diagnostic methods entirely; they are often used in conjunction with other tests to provide a comprehensive assessment of gut health. Considering food rituals that help your gut feel safe and steady alongside diagnostic tools provides holistic care.
Understanding Gut Scan Technologies
There isn’t one single “gut scan.” The term encompasses several different imaging modalities, each with its strengths and weaknesses. Choosing the appropriate scan depends on what clinicians are looking for. Some common technologies include: – Capsule Endoscopy: A tiny wireless camera is swallowed by the patient and travels through the digestive tract, transmitting images back to a recorder. This is excellent for visualizing the small intestine, which is difficult to reach with colonoscopies. – CT Enterography: Uses computed tomography (CT) scans combined with oral contrast agents to visualize the small bowel in detail. It’s particularly useful for detecting inflammation, strictures, and tumors. – MRI Enteroclysis: Similar to CT enterography but uses magnetic resonance imaging (MRI), avoiding radiation exposure. Often preferred for patients who need repeated scans or are sensitive to radiation. – Breath Tests: While not strictly an “imaging” scan, hydrogen breath tests can identify issues like Small Intestinal Bacterial Overgrowth (SIBO) by measuring gases produced during digestion.
The selection of a specific gut scan is driven by the patient’s symptoms and suspected underlying condition. For example, if a patient presents with unexplained abdominal pain and diarrhea, CT enterography or MRI enteroclysis might be recommended to investigate potential inflammatory bowel disease. If the concern centers around bleeding in the small intestine, capsule endoscopy would likely be the preferred method. The key is that these scans allow doctors to move beyond symptom management and address the underlying cause of gut issues. They provide a level of detail previously unavailable, making diagnosis more accurate and efficient. Furthermore, advancements in image processing and artificial intelligence are continually improving the sensitivity and specificity of these technologies. Establishing daily rhythms that help synchronize gut function can complement diagnostic insights.
These advanced imaging techniques often help rule out more serious organ complications, such as Crohn’s disease, ulcerative colitis, celiac disease, tumors (both benign and malignant), intestinal obstructions, and vascular abnormalities. They can also identify subtle signs of malabsorption or inflammation that might be missed with conventional testing. The ability to visualize the entire digestive tract, from the esophagus to the rectum, is a significant advantage over traditional methods.
Ruling Out Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease – encompassing Crohn’s disease and ulcerative colitis – presents diagnostic challenges due to its varied symptoms and potential for subtle presentation. Gut scans play an increasingly vital role in early detection and accurate diagnosis of IBD. – CT Enterography and MRI Enteroclysis are particularly effective at identifying inflammation, thickening of the bowel wall, and fistulas (abnormal connections between organs) – hallmarks of Crohn’s disease. – Capsule Endoscopy can detect inflammation in the small intestine, which is often affected by Crohn’s but difficult to assess with colonoscopy alone.
Traditionally, diagnosing IBD required multiple colonoscopies and biopsies, which were invasive and sometimes failed to identify early-stage disease. Gut scans provide a non-invasive alternative that can accurately visualize the extent and severity of inflammation. This allows doctors to make more informed treatment decisions and monitor the patient’s response to therapy. Early diagnosis is crucial in IBD, as it allows for prompt initiation of treatment, which can help prevent complications and improve long-term outcomes. Gut scans contribute significantly to this early detection process.
Moreover, gut scans are invaluable in differentiating between Crohn’s disease and ulcerative colitis – two distinct conditions with different management strategies. While both involve inflammation, they affect different parts of the digestive tract. The scan images allow clinicians to pinpoint the location and nature of the inflammation, leading to a more accurate diagnosis and tailored treatment plan. Understanding how the vagus nerve regulates gas and gut movement provides further context for IBD management.
Identifying Small Intestinal Issues
The small intestine has historically been the “blind spot” in gastroenterological diagnostics. It’s difficult to reach with conventional methods like colonoscopy, making it challenging to diagnose issues within this critical part of the digestive system. Gut scans, particularly capsule endoscopy and CT enterography, have revolutionized the assessment of small intestinal health. – Capsule endoscopy allows for direct visualization of the entire small intestine, detecting abnormalities such as ulcers, polyps, tumors, and bleeding sources. – CT Enterography can identify strictures (narrowing of the bowel), inflammation, and malabsorption issues within the small intestine.
Conditions like Small Intestinal Bacterial Overgrowth (SIBO) – where excessive bacteria accumulate in the small intestine – are often difficult to diagnose without specialized testing. While breath tests are commonly used for SIBO diagnosis, gut scans can help identify underlying structural abnormalities that may contribute to bacterial overgrowth. Identifying these issues is crucial because untreated SIBO can lead to malabsorption, bloating, and abdominal pain. The ability to visualize the small intestine with such clarity represents a major advancement in gastroenterological diagnostics.
Furthermore, gut scans are essential for diagnosing conditions like celiac disease – an autoimmune disorder triggered by gluten consumption. While blood tests can detect antibodies associated with celiac disease, gut scans can assess the degree of intestinal damage caused by gluten exposure and rule out other potential causes of similar symptoms.
Detecting Tumors and Obstructions
The early detection of tumors in the digestive tract is critical for improving survival rates. Gut scans provide a powerful tool for identifying both benign and malignant tumors. – CT Enterography and MRI Enteroclysis are highly sensitive for detecting tumors in the small intestine, while capsule endoscopy can identify polyps and small tumors throughout the digestive tract. – Colonoscopy remains the gold standard for detecting colon cancer, but gut scans can help identify areas of concern that warrant further investigation with a colonoscopy.
Beyond tumor detection, gut scans are also invaluable for identifying intestinal obstructions – blockages that prevent food from passing through the digestive tract. These obstructions can be caused by tumors, adhesions (scar tissue), or inflammation. Prompt diagnosis and treatment of an obstruction are essential to prevent serious complications. Gut scans allow clinicians to quickly identify the location and cause of the obstruction, guiding surgical intervention if necessary. It’s also helpful to know how to naturally support gut transit and reduce pressure for overall digestive health.