The intricate relationship between thyroid function and overall health is increasingly recognized, extending far beyond metabolic rate regulation. Many individuals with thyroid disorders – whether hypothyroidism (underactive thyroid) or hyperthyroidism (overactive thyroid) – experience significant gastrointestinal (GI) disturbances. These aren’t merely secondary symptoms; they represent a complex interplay where the thyroid hormone directly and indirectly impacts gut motility, microbiome composition, nutrient absorption, and even intestinal permeability. Ignoring these GI issues can hinder treatment efficacy for the thyroid condition itself and profoundly affect quality of life. Understanding this connection is crucial for holistic patient care, moving beyond simply addressing thyroid hormone levels to supporting overall digestive wellness.
The conventional approach often focuses on restoring optimal thyroid hormone levels through medication or other interventions. While vital, this isn’t always enough. The gut’s health can influence how the body utilizes those hormones and also contribute significantly to the symptoms people experience – fatigue, brain fog, weight fluctuations, even mood disturbances – that are frequently associated with thyroid dysfunction. This bidirectional relationship highlights the need for comprehensive evaluation of gut function in individuals diagnosed with any form of thyroid disease, as well as those presenting with unexplained GI symptoms alongside potential thyroid concerns. It’s a move towards understanding the root causes rather than just managing the effects.
The Thyroid-Gut Axis: A Two-Way Street
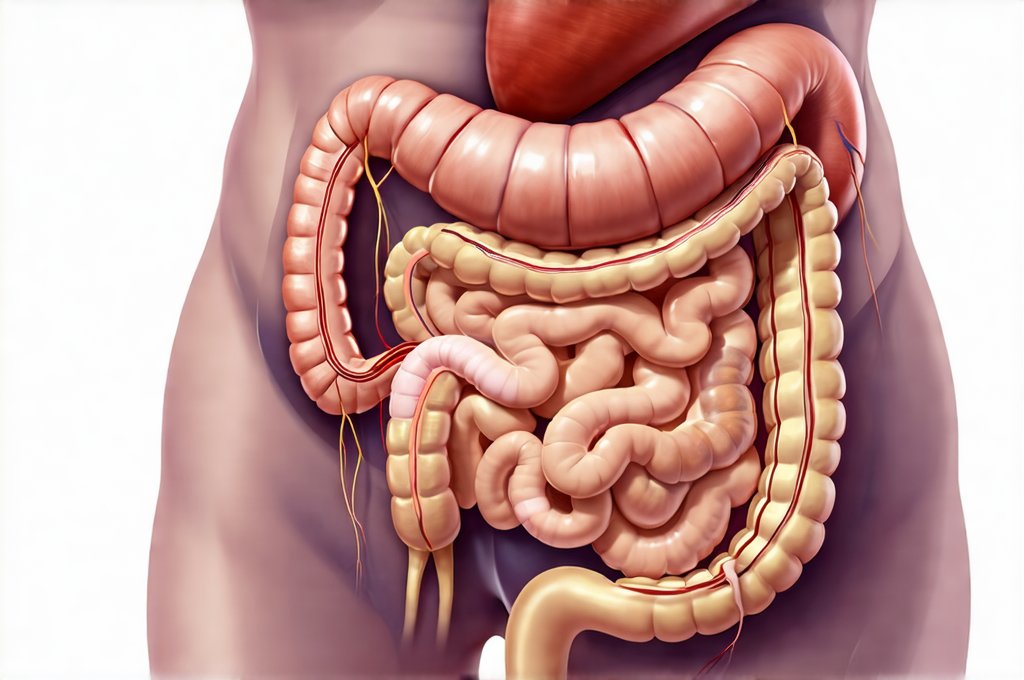
The connection between the thyroid and the gut isn’t a one-way street; it’s an axis where each system profoundly influences the other. Thyroid hormones, particularly T3 (triiodothyronine), directly affect gut motility. Hypothyroidism slows down digestion, leading to constipation, bloating, and abdominal discomfort – very common complaints among those with underactive thyroids. Conversely, hyperthyroidism can accelerate gut transit time, resulting in diarrhea or loose stools. But the impact goes deeper than just speed. Thyroid hormone also influences the structure and function of the intestinal cells themselves, affecting nutrient absorption and potentially increasing intestinal permeability—often referred to as “leaky gut.” The Role of Gut Permeability is a key factor in this process.
The gut microbiome – the trillions of bacteria residing within our digestive tract – plays a critical role in this axis. Thyroid hormones can influence the composition of the gut microbiome, and conversely, the microbiome impacts thyroid hormone conversion. A significant portion of T4 (thyroxine), the inactive form of thyroid hormone, needs to be converted into the active T3 by enzymes called deiodinases. Certain gut bacteria contribute to this process, while others can interfere with it or even produce substances that disrupt thyroid hormone function. An imbalanced microbiome – dysbiosis – can therefore exacerbate thyroid issues and make them more difficult to manage. Furthermore, inflammation within the gut, often driven by dysbiosis, can impair thyroid hormone production and utilization. Finding Humor in the Chaos can help cope with the frustrations of a disrupted microbiome.
Finally, autoimmune thyroid conditions like Hashimoto’s thyroiditis and Graves’ disease are strongly linked to intestinal health. A significant percentage of individuals with these conditions also experience increased intestinal permeability, allowing undigested food particles and toxins to enter the bloodstream, triggering an immune response that can worsen both gut and thyroid inflammation. Addressing gut health may therefore play a crucial role in modulating autoimmune activity and improving overall outcomes for those with autoimmune thyroid disease. Compassion Practices are invaluable when navigating the challenges of autoimmune conditions.
Evaluating Gut Function: Key Assessment Tools
Assessing gut function isn’t just about identifying specific symptoms; it requires a multi-faceted approach. A thorough patient history is the starting point, focusing on detailed questions about bowel habits (frequency, consistency, urgency), bloating, gas, abdominal pain, and any associated dietary triggers or sensitivities. It’s important to inquire about past antibiotic use, stress levels, and other factors that can impact the gut microbiome. Physical examination should include palpation of the abdomen to assess for tenderness or distention. However, these subjective assessments are often insufficient; objective testing is crucial for a comprehensive evaluation.
Several tests can provide valuable insights into gut function. Stool testing, particularly advanced functional stool analysis, offers detailed information about microbiome composition (identifying beneficial and pathogenic bacteria), markers of inflammation, digestive enzyme production, and intestinal permeability (assessed through markers like zonulin). Breath tests can detect small intestinal bacterial overgrowth (SIBO), a common condition where excessive bacteria reside in the small intestine, interfering with nutrient absorption. Food sensitivity testing – though controversial – may help identify potential dietary triggers contributing to gut inflammation. It’s important to remember that no single test provides a complete picture; integrating results from multiple assessments is essential for accurate diagnosis and targeted interventions.
Beyond stool and breath tests, assessing nutrient status is crucial, especially for those with thyroid dysfunction. Deficiencies in vitamins D, B12, iron, zinc, and selenium are common in both hypothyroidism and hyperthyroidism, impacting gut health and overall well-being. Blood tests can identify these deficiencies, allowing for targeted supplementation if necessary. Finally, considering markers of inflammation – such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) – can help assess the degree of gut and systemic inflammation present. This holistic approach ensures a comprehensive understanding of the patient’s gut health status. High-Satiety Meals can support nutrient absorption.
Dietary Interventions for Gut Support in Thyroid Conditions
Diet plays a pivotal role in supporting gut function, particularly for individuals with thyroid issues. A foundational step is often adopting an anti-inflammatory diet, rich in whole, unprocessed foods and minimizing processed foods, sugar, and refined carbohydrates. Increasing fiber intake (from sources like vegetables, fruits, and gluten-free grains) can promote healthy bowel movements and support a diverse microbiome – but this needs to be done cautiously, as too much fiber too quickly can exacerbate bloating in some individuals. Focusing on gut-healing nutrients is also essential.
Specific dietary strategies may vary depending on the thyroid condition and individual sensitivities. For example, those with Hashimoto’s often benefit from a gluten-free diet, even without a formal diagnosis of celiac disease, as gluten can trigger autoimmune activity. Elimination diets – carefully removing potential food triggers for a period of time and then reintroducing them one by one to assess tolerance – can help identify sensitivities. Probiotic-rich foods like yogurt (if tolerated), kefir, sauerkraut, and kimchi can support microbiome diversity, but supplementation may be necessary in some cases. Finally, addressing nutrient deficiencies through targeted supplementation is crucial.
It’s vital to avoid restrictive diets that eliminate entire food groups without proper guidance from a healthcare professional. Personalized nutrition is key – what works for one person may not work for another. A registered dietitian or functional medicine practitioner can help develop a tailored dietary plan based on individual needs and sensitivities, ensuring adequate nutrient intake while supporting gut health and thyroid function. Remember that dietary changes are most effective when combined with other lifestyle modifications like stress management and regular exercise.
The Role of Lifestyle Factors & Future Directions
Beyond diet and testing, several lifestyle factors significantly influence gut health and its interaction with the thyroid. Stress management is paramount. Chronic stress can disrupt the gut microbiome, increase intestinal permeability, and negatively impact thyroid hormone conversion. Techniques like mindfulness, yoga, meditation, and deep breathing exercises can help mitigate stress levels. Regular physical activity also supports gut motility, reduces inflammation, and improves overall health. Adequate sleep is essential for restoring gut function and supporting a healthy immune system. GERD in People with Desk Jobs highlights the impact of lifestyle choices.
Emerging research is exploring the potential of fecal microbiota transplantation (FMT) – transferring fecal matter from a healthy donor to restore microbiome diversity – as a treatment option for autoimmune thyroid disease and other conditions linked to gut dysbiosis. Personalized probiotics, tailored to an individual’s specific microbiome profile, are also showing promise. Furthermore, the development of more sophisticated diagnostic tools for assessing gut function will continue to refine our understanding of this complex relationship.
Ultimately, evaluating gut function is no longer a peripheral consideration in thyroid care; it’s becoming increasingly recognized as an integral part of holistic treatment. By addressing both thyroid hormone levels and gut health, healthcare practitioners can optimize patient outcomes and improve quality of life for those living with thyroid disorders. A collaborative approach – involving physicians, registered dietitians, and functional medicine practitioners – is essential for delivering comprehensive and personalized care that addresses the root causes of illness rather than simply managing symptoms. Helping Kids Navigate Birthday Parties demonstrates how to support those with gut issues in daily life.