Colitis, an inflammation of the colon, can significantly disrupt daily life when it flares up. While initial treatment often focuses on managing the acute symptoms – reducing inflammation and alleviating discomfort – the period following a flare is crucial for long-term management, preventing recurrence, and restoring overall well-being. This phase isn’t simply about waiting for things to return to normal; it’s an active process of monitoring, adjustment, and proactive care tailored to the individual’s specific situation. Understanding what tools are available for effective follow-up is empowering, allowing patients to take control of their health journey and collaborate effectively with healthcare professionals.
The aftermath of a colitis flare can present unique challenges. Individuals may experience lingering symptoms like abdominal discomfort, altered bowel habits, fatigue, or nutritional deficiencies. The psychological impact shouldn’t be underestimated either; flares can cause anxiety about future episodes and disrupt social activities. Therefore, follow-up isn’t solely medical – it encompasses lifestyle adjustments, dietary modifications, and mental health support. A comprehensive approach is vital for rebuilding strength, minimizing the risk of relapse, and improving quality of life. This article explores key tools used after a flare of colitis to help navigate this important phase.
Monitoring & Assessment Tools
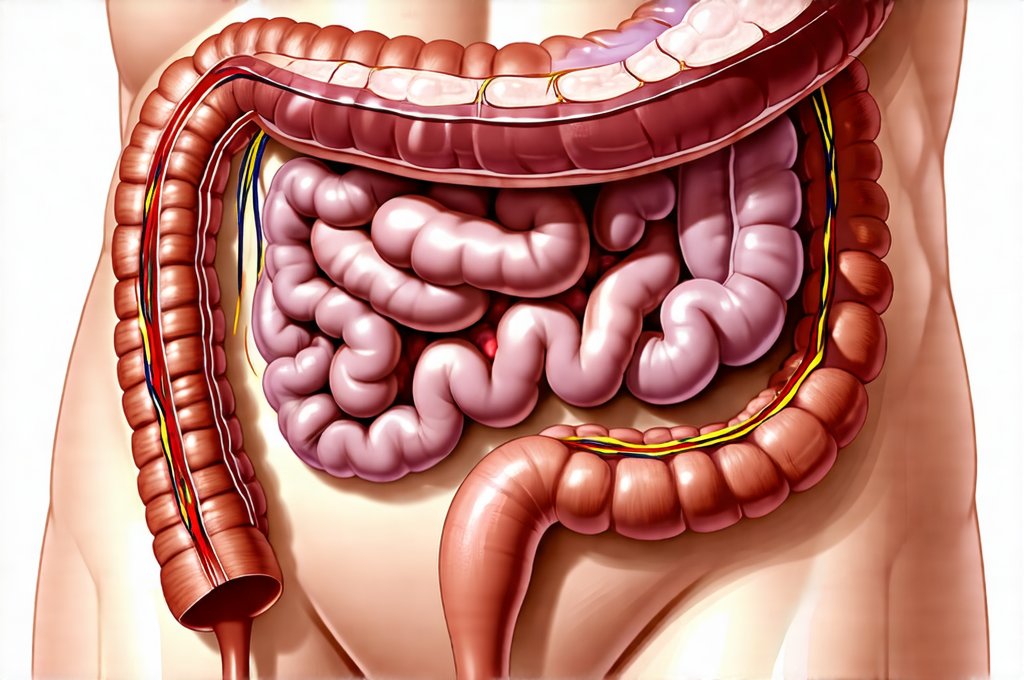
Effective follow-up begins with consistent monitoring to assess how well the colon is healing and to identify any early signs of recurrence. This involves a combination of clinical assessments performed by your healthcare provider, alongside self-monitoring techniques you can implement at home. Regular communication with your gastroenterologist or primary care physician is paramount throughout this process. Several objective measurements are often employed. Fecal calprotectin tests, for example, measure inflammation in the colon and can be a sensitive indicator of disease activity even when symptoms are mild. Colonoscopies, though more invasive, remain the gold standard for evaluating the extent of healing and detecting any complications. Blood tests help assess nutritional status (particularly iron levels often depleted during flares) and monitor inflammatory markers.
Beyond these clinical assessments, keeping a detailed symptom diary can be incredibly valuable. This diary should record: – Frequency of bowel movements – Stool consistency (using a Bristol stool chart is helpful) – Severity of abdominal pain or discomfort – Any associated symptoms like fatigue, nausea, or loss of appetite – Dietary intake – what you ate and when – Stress levels and any triggering events This information provides your healthcare team with invaluable insights into your individual disease course and helps tailor treatment adjustments. It also empowers you to recognize patterns and potential triggers. If you are struggling after overeating, consider evening gut reset meals to ease symptoms.
Finally, quality-of-life questionnaires are increasingly used in colitis management. These questionnaires assess the impact of the condition on various aspects of daily life, including physical function, emotional well-being, social activities, and relationships. This holistic approach ensures that treatment isn’t solely focused on reducing inflammation but also on improving overall quality of life. It helps to identify areas where additional support or interventions might be needed. Understanding how to reset your gut can greatly assist in this process.
Dietary Management & Nutritional Support
Diet plays a significant role in both triggering flares and supporting recovery. There’s no one-size-fits-all diet for colitis; individual tolerances vary greatly. However, certain principles are generally recommended during the follow-up period. A low-residue diet – limiting high-fiber foods – is often advised initially to allow the colon to rest and heal. This means reducing intake of whole grains, raw fruits and vegetables, nuts, and seeds. As symptoms improve, foods can be gradually reintroduced one at a time to identify potential triggers. Food diaries are particularly helpful during this process. It’s important to know why you may feel bloated so you can adjust your diet accordingly.
Nutritional deficiencies are common after flares, especially iron deficiency anemia due to blood loss. Supplementation may be necessary based on blood test results. Adequate hydration is also crucial, as diarrhea and inflammation can lead to dehydration. A registered dietitian specializing in gastrointestinal disorders can provide personalized dietary guidance tailored to your specific needs and tolerances. They can help you identify nutrient-rich foods that are well-tolerated and develop a sustainable long-term eating plan. It’s important to remember that restrictive diets should be avoided whenever possible, as they can negatively impact nutritional status and quality of life. Consider foundations of an evening routine for optimal gut health.
Furthermore, exploring the role of probiotics and prebiotics is becoming increasingly common. Probiotics – live microorganisms found in fermented foods or supplements – may help restore gut microbiome balance. Prebiotics – non-digestible fibers that feed beneficial bacteria – can also support a healthy gut environment. However, it’s crucial to discuss these options with your healthcare provider, as they aren’t suitable for everyone and may even exacerbate symptoms in some individuals. If you are struggling after a flare, learning how to recover is vital.
Psychological Support & Stress Management
Colitis can have a profound psychological impact. Living with a chronic illness that causes unpredictable flares can lead to anxiety, depression, social isolation, and fear of recurrence. It’s essential to address these emotional challenges as part of your overall follow-up plan. Psychotherapy – such as cognitive behavioral therapy (CBT) or mindfulness-based stress reduction (MBSR) – can provide coping strategies for managing anxiety and improving emotional well-being. Support groups, both in-person and online, offer a sense of community and allow you to connect with others who understand your experiences.
Stress is a known trigger for colitis flares in many individuals. Learning effective stress management techniques is therefore crucial. These might include: – Regular exercise – even gentle activities like walking or yoga can help reduce stress levels – Meditation or mindfulness practices – Deep breathing exercises – Spending time in nature – Engaging in hobbies and activities you enjoy – Prioritizing sleep Developing a strong social support network can also buffer against the negative effects of stress.
Finally, don’t hesitate to seek professional mental health support if you’re struggling with anxiety or depression. Your healthcare provider can refer you to a qualified therapist or psychiatrist who specializes in chronic illness management. Prioritizing your mental health is just as important as managing your physical symptoms. It’s about holistic care and building resilience for the long term. If experiencing digestive issues after heavy meals, learn how to ease digestive symptoms.