The modern world often feels like a relentless pressure cooker. Demanding jobs, constant connectivity, financial worries, relationship strains – all contribute to chronic stress for many individuals. While we often focus on mental and emotional impacts, the digestive system is profoundly affected by stress, creating a vicious cycle where gut issues exacerbate stress levels and vice versa. Many people living high-stress lifestyles experience symptoms like bloating, constipation, diarrhea, heartburn, or even more serious conditions like Irritable Bowel Syndrome (IBS). Ignoring these signals can lead to long-term health problems and diminished quality of life. Understanding the link between stress and digestion is the first step toward regaining control, and a powerful tool for achieving that understanding is digestive tracking.
Digestive tracking isn’t about restrictive dieting or obsessive calorie counting; it’s about mindful self-awareness. It’s a process of systematically recording what you eat, how your body responds, and factoring in the context of your stress levels and daily activities. This allows you to identify personal triggers – foods that consistently cause discomfort, stress patterns linked to digestive upset, or lifestyle factors playing a role. It’s about gathering data to inform more conscious choices and ultimately cultivate a healthier relationship with food and your body. Think of it as detective work for your gut—uncovering the clues needed to restore balance. This isn’t a quick fix; it’s an ongoing practice that empowers you to become an active participant in your own wellbeing. You might find food journal prompts helpful as you begin this process.
The Stress-Digestion Connection: A Deeper Look
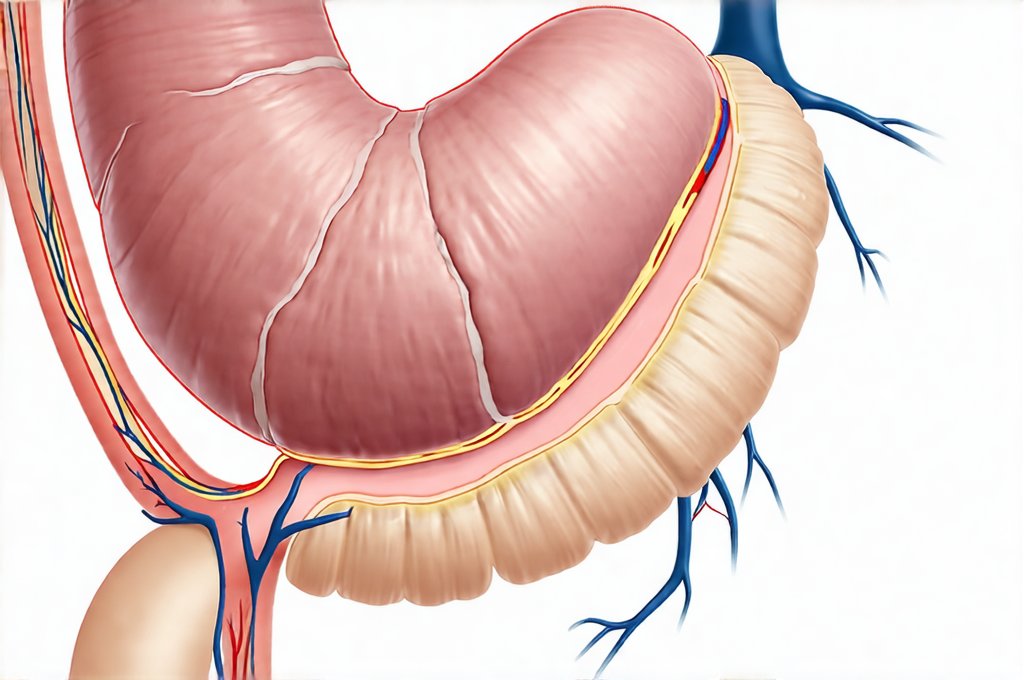
The connection between stress and digestion is far more than just “nervous stomach”. It’s rooted in the gut-brain axis, a bidirectional communication network linking the digestive system to the brain. When you experience stress, your body initiates the “fight or flight” response, releasing hormones like cortisol. While essential for survival in acute situations, chronic activation of this system disrupts normal digestive function. Blood flow is diverted away from the gut and toward muscles preparing for action, slowing down digestion and potentially leading to issues like constipation. Simultaneously, increased intestinal permeability (often called “leaky gut”) can occur, allowing undigested food particles and toxins to enter the bloodstream, further fueling inflammation and impacting overall health.
This disruption manifests differently in everyone. Some individuals experience a speeding up of digestive processes – leading to diarrhea or urgency – while others become severely constipated as their system essentially shuts down. Stress also influences gut motility (the movement of food through your digestive tract) and visceral hypersensitivity (increased sensitivity to pain in the gut). This means that even normal amounts of gas or bowel movements can feel intensely uncomfortable during times of stress. Furthermore, cortisol impacts the microbiome – the trillions of bacteria living in our gut – potentially reducing beneficial bacteria and promoting the growth of harmful ones. A compromised microbiome further weakens digestion and immune function, creating a downward spiral.
It’s important to recognize that stress isn’t always obvious. It can be subtle—a constant low-level anxiety about work deadlines, worrying about finances, or feeling overwhelmed by social obligations. These seemingly minor stressors accumulate over time and have a significant impact on the digestive system. This is where digestive tracking comes in – helping you identify these patterns and understand how your body responds to different levels of stress. Prioritizing compassion practices can also be invaluable during challenging times.
What to Track: Building Your Digestive Diary
Effective digestive tracking isn’t about recording every single detail, but rather focusing on key elements that provide meaningful insights. Begin with a dedicated notebook or utilize one of the many available apps designed for this purpose (there are numerous options ranging from simple note-taking apps to specialized gut health trackers). The core components you should track include: – What you eat and drink (be specific – include ingredients, portion sizes, and method of preparation) – When you ate/drank it – Your digestive symptoms (bloating, gas, heartburn, constipation, diarrhea, stomach pain, nausea, etc.) including severity on a scale of 1-10. – Your stress levels (on a scale of 1-10 or using descriptive terms like “low,” “moderate,” “high”) and the source of your stress – Any relevant activities (exercise, travel, sleep quality) – these can all impact digestion.
Be consistent! The more diligently you track, the more accurate your data will be. Don’t skip days, even if you feel good. Tracking on “good” days is just as important as tracking on bad days because it helps identify what supports healthy digestion. Aim to record your information shortly after eating or experiencing symptoms to ensure accuracy. Consider adding a section for “emotional state” – how were you feeling emotionally before and during meals? Emotions can significantly influence both food choices and digestive processes. Remember, this isn’t about self-judgment; it’s about gathering information. Avoid labeling foods as “good” or “bad.” Focus on how they make you feel.
Identifying Your Personal Triggers
Once you’ve been tracking for a week or two, start looking for patterns. Are there specific foods that consistently cause discomfort? Do stress levels seem to exacerbate certain symptoms? For example, do you notice bloating after consuming dairy when you’re feeling particularly anxious about work? Or does constipation worsen during periods of high travel and disrupted sleep? Look beyond the obvious culprits. Sometimes seemingly harmless foods can trigger issues based on individual sensitivities or combinations with other factors.
Don’t immediately eliminate entire food groups without further investigation. Instead, consider experimenting with smaller portions or different preparations to see if that makes a difference. For example, if you suspect lactose intolerance, try incorporating dairy alternatives or using lactase enzyme supplements. Also, pay attention to the timing of your meals. Eating large meals close to bedtime can disrupt digestion, especially when stressed. Consider breaking up larger meals into smaller, more frequent snacks throughout the day.
Stress Management and Digestive Health
Digestive tracking isn’t just about food; it’s about understanding how stress impacts your gut. If you notice a strong correlation between high stress levels and digestive upset, prioritize stress management techniques. This could include: – Mindfulness meditation – even 5-10 minutes daily can make a difference. – Deep breathing exercises – simple yet effective for calming the nervous system. – Regular exercise – releases endorphins and reduces stress hormones. – Spending time in nature – proven to lower cortisol levels. – Practicing gratitude – shifting your focus to positive aspects of life.
Experiment with different techniques to find what works best for you. Don’t try to implement everything at once; start small and gradually incorporate new practices into your routine. Consider journaling alongside your digestive tracking, exploring the root causes of your stress and identifying coping mechanisms that work effectively. Remember that seeking support from a therapist or counselor can also be incredibly beneficial in managing chronic stress. Acknowledging and addressing the underlying emotional factors contributing to your stress is crucial for long-term digestive health. If you find yourself struggling on particularly difficult days, consider supportive food choices to ease discomfort.
Refining Your Approach: Long-Term Sustainability
Digestive tracking isn’t a one-time project; it’s an ongoing process of self-discovery. As you learn more about your body, refine your approach and adjust your dietary and lifestyle choices accordingly. Over time, you may find that you need to track less frequently as you develop a deeper understanding of your triggers and responses. The goal isn’t to become obsessed with tracking but to cultivate a mindful awareness of how food and stress impact your wellbeing.
Continue to revisit your data periodically to identify new patterns or changes in your body’s response to different stimuli. Be patient and compassionate with yourself – digestive health is complex, and progress may not always be linear. Focus on making small, sustainable changes that you can maintain over the long term. Remember that you are the expert on your own body, and digestive tracking empowers you to take control of your health and create a life that feels both nourishing and fulfilling. Understanding potential sensitivities, like to citric acid, can also be valuable in this process.