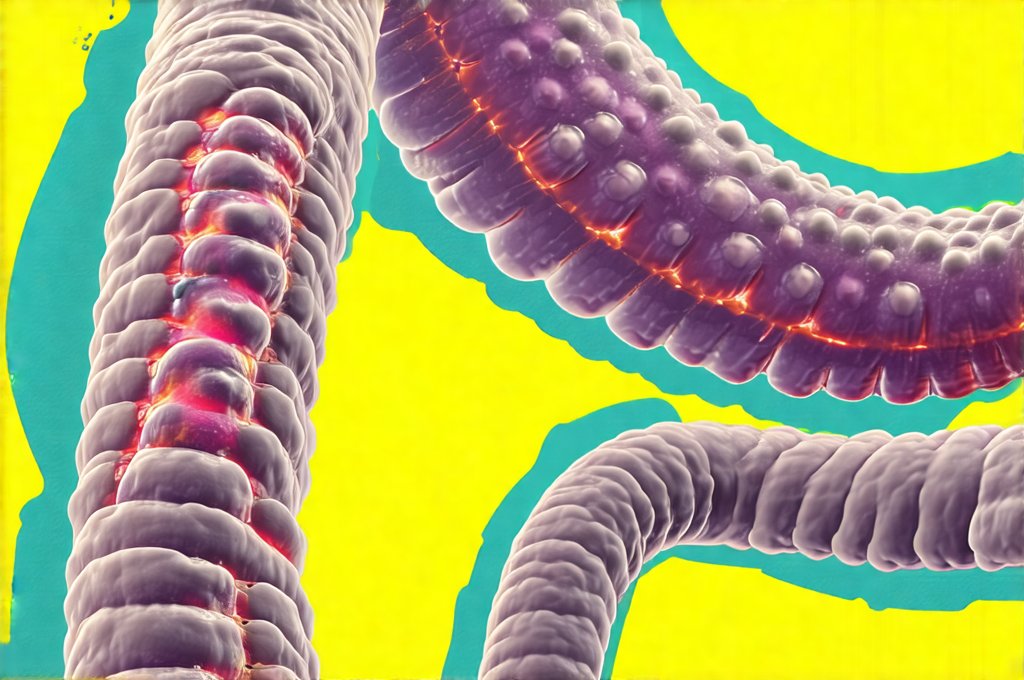
Our bodies are ecosystems, teeming with trillions of microorganisms – bacteria, fungi, viruses, and archaea – collectively known as the microbiome. This complex community resides primarily in our gut but extends to skin, mouth, lungs, and other areas. For years, these microscopic inhabitants were largely ignored, but emerging research reveals their profound influence on nearly every aspect of health, from digestion and immunity to mental wellbeing and even chronic disease risk. Understanding your microbiome isn’t about chasing a “perfect” microbial profile; it’s about gaining insights into how your unique ecosystem functions and identifying potential areas for improvement through lifestyle adjustments or targeted interventions.
The growing accessibility of at-home microbiome testing kits has sparked considerable interest, but also confusion. Should everyone rush to test their gut flora? The answer isn’t straightforward. While these tests can provide valuable information for some, they aren’t necessarily beneficial – or even accurate – for all. This article will explore the circumstances where microbiome testing might be worthwhile, what you can realistically expect from it, and how to interpret results responsibly. We’ll also delve into the limitations of current testing methods and discuss alternative strategies for supporting a healthy gut microbiome without relying solely on test data.
When Might Microbiome Testing Be Useful?
Microbiome testing isn’t a one-size-fits-all solution. Its utility varies depending on individual circumstances and health goals. Consider testing if you’re experiencing persistent, unexplained symptoms that could be linked to gut health or if you’re proactively seeking ways to optimize your wellbeing based on personalized data. However, it’s crucial to manage expectations; a microbiome test isn’t typically diagnostic in the traditional sense, meaning it won’t definitively tell you what ails you. Instead, it offers a snapshot of microbial composition that can inform lifestyle choices and potentially guide targeted interventions under professional guidance.
Specifically, individuals facing ongoing digestive issues such as bloating, gas, diarrhea, or constipation – even after consulting with a healthcare provider – might find testing helpful. It could help identify imbalances associated with these symptoms. Similarly, those with autoimmune conditions, allergies, skin problems like eczema, or mental health concerns (given the gut-brain axis) may explore testing to understand potential links between their microbiome and their condition. People who have recently completed a course of antibiotics – which can disrupt the microbial balance – might also consider testing to assess recovery and support repopulation with beneficial bacteria. If you are concerned about ongoing digestive issues, it’s important to know if your bloating is lymphatic or digestive in nature. However, it’s important to note that correlation doesn’t equal causation. Even if a test reveals an imbalance, it doesn’t automatically mean this imbalance is causing your symptoms. Other factors could be at play, and further investigation may be needed. Also, remember that microbiome composition is incredibly dynamic – influenced by diet, stress, sleep, medications, and many other variables – so a single snapshot provides limited information. If you’re concerned about the reasons behind consistent discomfort, consider how to tell if your gas is a sign of something more serious.
Understanding the Limitations of Microbiome Testing
While promising, current microbiome testing technologies aren’t without their limitations. Most at-home tests primarily analyze bacteria using 16S rRNA gene sequencing, which identifies microbial species but doesn’t necessarily reflect their function. It tells you who is there, but not what they are doing. This means a test might identify the presence of potentially harmful bacteria, but it can’t determine if those bacteria are actively producing toxins or causing inflammation. More advanced (and expensive) techniques like metagenomic sequencing offer insights into microbial function, but these aren’t widely available in at-home kits.
Another limitation is standardization and interpretation. Different testing companies use different methods for collecting samples, analyzing data, and reporting results. This can lead to inconsistencies and makes it difficult to compare results across labs. Furthermore, interpreting the “normal” range for microbial abundance is challenging. There’s no universally agreed-upon ideal microbiome profile; diversity and composition vary widely among individuals based on genetics, environment, and lifestyle. Many tests provide recommendations based on broad population averages, which may not be relevant to your specific needs.
Finally, it’s crucial to understand that the microbiome is a complex ecosystem, and testing only captures a small portion of this complexity. Tests often focus on bacteria while overlooking other important microorganisms like fungi, viruses, and archaea. Relying solely on test results without considering other health factors or seeking professional guidance can lead to misinterpretations and potentially misguided interventions.
Navigating Test Results & Actionable Steps
If you decide to pursue microbiome testing, understanding how to navigate the results is essential. First, choose a reputable testing company that clearly explains its methodology, data analysis process, and limitations. Look for tests that provide detailed reports with actionable insights rather than just raw data. Avoid companies that make exaggerated claims or promise quick fixes.
Once you receive your results, resist the urge to self-diagnose or drastically alter your diet based solely on the report. Instead, consult with a qualified healthcare professional – such as a registered dietitian specializing in gut health or a functional medicine practitioner – who can help you interpret the findings and develop a personalized plan. Here’s how to approach the process:
- Focus on trends: Look for overall patterns rather than fixating on individual microbial abundances. Are there significant imbalances? Is diversity low?
- Consider your symptoms: Relate the test results back to your specific health concerns. Does the report align with your experience?
- Prioritize lifestyle changes: The most effective way to improve microbiome health is often through sustainable lifestyle adjustments:
- Diet: Increase fiber intake, incorporate fermented foods, and reduce processed foods, sugar, and artificial sweeteners.
- Stress management: Practice techniques like mindfulness, yoga, or meditation.
- Sleep: Aim for 7-9 hours of quality sleep per night.
- Exercise: Engage in regular physical activity. To better understand your body’s signals, it can be useful to know how long should you wait to lie down after eating.
Beyond Testing: Supporting Gut Health Naturally
Even without microbiome testing, there are numerous ways to support a healthy gut microbiome. Prioritizing whole foods, particularly those rich in fiber (fruits, vegetables, legumes, and whole grains), is fundamental. Fiber serves as food for beneficial bacteria, promoting their growth and diversity. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha contain live microorganisms that can contribute to a healthier gut ecosystem – but start slowly to avoid digestive upset.
Prebiotics – non-digestible fibers that feed beneficial bacteria – are also crucial. Good sources include garlic, onions, leeks, asparagus, bananas, and oats. Reducing intake of processed foods, sugar, artificial sweeteners, and excessive alcohol consumption can minimize disruption to the microbiome. Antibiotic use should be reserved for necessary medical conditions, as they indiscriminately kill both beneficial and harmful bacteria. If you’re experiencing ongoing issues like abdominal bloating, it’s important to understand if your abdominal bloating is due to water retention.
The Future of Microbiome Analysis & Personalized Nutrition
The field of microbiome research is rapidly evolving. Advances in technologies like metagenomic sequencing and metabolomics are providing a more comprehensive understanding of microbial function and interactions with the host. This will lead to more accurate and personalized testing methods, enabling tailored interventions based on individual microbial profiles.
Personalized nutrition – dietary recommendations based on an individual’s genetic makeup, microbiome composition, and lifestyle factors – is poised to become increasingly prevalent. In the future, we may see microbiome testing integrated into routine healthcare screenings, allowing for early detection of imbalances and proactive strategies for preventing chronic disease. However, it’s important to remember that the microbiome isn’t the sole determinant of health. It interacts with a complex network of genetic, environmental, and lifestyle factors. A holistic approach – combining personalized insights from microbiome analysis with comprehensive healthcare assessments – will be key to unlocking the full potential of this fascinating field. Learning how to know if your gut is healing can also provide valuable feedback during this process, and help you understand how to tell if you’re really improving. Lastly, understanding how to tell if your reflux is acidic or non-acidic can help you refine your approach to gut health.