Bloating is an incredibly common complaint, affecting millions worldwide. It’s often dismissed as simply “part of life,” something we endure after indulging in certain foods or experiencing stress. However, persistent bloating can be a sign of underlying issues, and one surprisingly frequent culprit is silent reflux, also known as laryngopharyngeal reflux (LPR). Unlike traditional heartburn where you experience burning sensations in the chest, silent reflux often presents with subtle, seemingly unrelated symptoms like chronic cough, sore throat, or…bloating. This makes it difficult to identify and address effectively, leading many people to suffer for years without understanding the root cause of their discomfort.
The insidious nature of silent reflux stems from its name – it’s silent because the typical warning signs are missing. Stomach acid travels up the esophagus, but instead of causing heartburn, it reaches higher into the throat and even nasal passages. This process can irritate these sensitive areas, leading to inflammation and a host of seemingly unrelated symptoms. Critically, this acidic backflow isn’t always about burning; it disrupts normal digestion and can significantly impact gut health, creating an environment ripe for bloating and other digestive disturbances. Understanding this connection is the first step towards finding relief. Recognizing the difference between these discomforts is key to proper treatment.
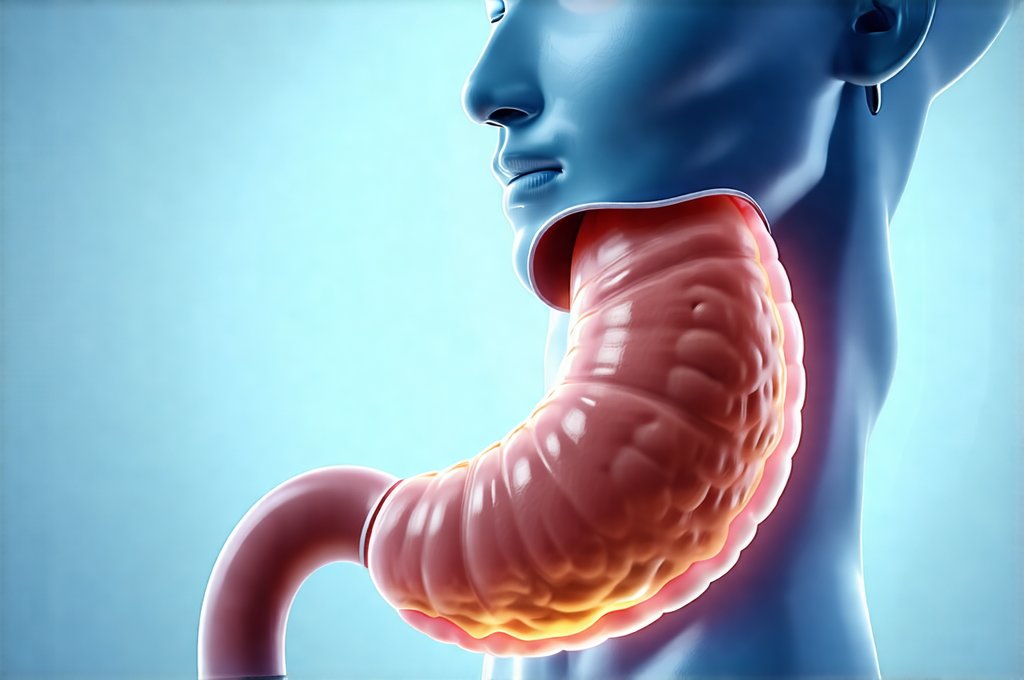
The Mechanics of Silent Reflux & Bloating
Silent reflux doesn’t just involve acid traveling upwards; it’s a complex interplay between several factors. A weakened lower esophageal sphincter (LES) – the muscle that normally prevents stomach contents from flowing back up – is often at the heart of the problem. This weakness can be caused by numerous things, including dietary habits, obesity, smoking, or even certain medications. When the LES isn’t functioning properly, acid escapes and begins its journey upwards. However, it’s not solely about how much acid refluxes; it’s also about what kind of material is involved. Silent reflux frequently includes a mix of stomach contents – acid, bile, enzymes, and partially digested food – that irritate the delicate tissues higher up in the digestive tract.
This chronic irritation triggers inflammation throughout the digestive system. The body attempts to neutralize the acidic backflow with bicarbonate secretions, but this process can disrupt normal gut motility (the movement of food through the digestive tract). Slower motility means food lingers longer in the stomach and intestines, providing more opportunity for gas production by bacteria. This leads to increased bloating, distension, and discomfort. Furthermore, inflammation itself can contribute to visceral hypersensitivity – an amplified perception of pain or discomfort in the gut – making even normal amounts of gas feel intensely uncomfortable. You might also experience frequent burping alongside these symptoms.
The connection isn’t always straightforward. Some individuals with silent reflux experience minimal esophageal symptoms but substantial bloating. This highlights that the location and impact of the reflux are more important than simply its presence. For example, acid reaching the duodenum (the first part of the small intestine) can directly interfere with nutrient absorption and exacerbate bloating by altering gut microbiome composition. It’s a cascading effect, where one issue leads to another, making diagnosis and treatment challenging. The relationship between acid reflux and bloating is often complex and requires careful examination.
Identifying Silent Reflux: Beyond Heartburn
Traditional GERD (gastroesophageal reflux disease) is usually diagnosed based on heartburn symptoms. However, silent reflux requires a different approach, as these classic signs are often absent or minimal. This makes self-diagnosis incredibly difficult. A key indicator is the presence of extraesophageal symptoms – those seemingly unrelated to the digestive system.
- Chronic cough: Particularly at night or after meals
- Hoarseness or voice changes
- Frequent throat clearing
- A sensation of a lump in the back of the throat (globus sensation)
- Postnasal drip
- Unexplained earaches
- Bloating, gas, and abdominal discomfort
If you experience several of these symptoms without heartburn, silent reflux should be considered. A gastroenterologist can perform diagnostic tests to confirm the diagnosis. These might include:
- Laryngoscopy: A visual examination of the larynx (voice box) to look for signs of inflammation or irritation.
- 24-hour pH monitoring: This involves placing a small capsule in your esophagus to measure acid levels over a 24-hour period. It’s considered the gold standard for diagnosing reflux, even silent reflux.
- Impedance testing: This measures both acid and non-acid reflux events, providing a more comprehensive picture of what’s happening in the esophagus.
It’s important to note that these tests aren’t always conclusive, and diagnosis often relies on a combination of symptoms, medical history, and response to treatment. Understanding acidic and alkaline reflux differences can help with accurate diagnosis too.
Dietary Considerations for Silent Reflux & Bloating
Diet plays a pivotal role in both managing silent reflux and reducing bloating. While there isn’t a one-size-fits-all diet, certain foods are known triggers for both conditions. Avoiding these can significantly alleviate symptoms. Common culprits include:
- Fatty and fried foods: These slow down digestion and increase acid production.
- Chocolate: Contains compounds that relax the LES.
- Caffeine: Can also weaken the LES and stimulate acid secretion.
- Alcohol: Similar effects to caffeine.
- Spicy foods: Can irritate the esophagus and stomach lining.
- Carbonated beverages: Introduce gas into the digestive system, exacerbating bloating.
- Mint: Surprisingly, mint can relax the LES, allowing for more reflux.
However, simply avoiding trigger foods isn’t enough. A proactive dietary approach focuses on incorporating gut-friendly foods that support healthy digestion and reduce inflammation.
- Fiber-rich foods: Fruits, vegetables, and whole grains promote regularity and prevent constipation, reducing bloating.
- Probiotic-rich foods: Yogurt, kefir, sauerkraut, and kimchi help balance gut bacteria, improving digestion and reducing gas production.
- Anti-inflammatory foods: Foods like turmeric, ginger, and omega-3 fatty acids (found in fish) can help reduce inflammation throughout the digestive system.
Eating smaller, more frequent meals can also help prevent overfilling the stomach and reducing pressure on the LES. Staying hydrated is crucial, but avoid drinking large amounts of water during meals, as this can dilute stomach acid and potentially worsen reflux. A link exists between gut pain and additives in food that should be considered too.
Lifestyle Adjustments & Long-Term Management
Dietary changes are only part of the equation. Lifestyle adjustments are equally important for managing silent reflux and minimizing bloating. One of the most impactful changes is elevating the head of your bed by 6-8 inches. This utilizes gravity to help keep stomach acid where it belongs – in the stomach – during sleep. Avoid eating within 2-3 hours of bedtime, allowing time for digestion before lying down.
Maintaining a healthy weight is also critical. Obesity increases pressure on the abdomen, forcing stomach contents upwards. Regular exercise can improve digestion and reduce stress, both of which contribute to bloating. Stress management techniques like yoga, meditation, or deep breathing exercises are also beneficial, as stress can exacerbate reflux symptoms.
Long-term management often involves a combination of lifestyle changes, dietary modifications, and potentially medication. Over-the-counter antacids can provide temporary relief, but they don’t address the underlying cause of the problem. Proton pump inhibitors (PPIs) or H2 blockers may be prescribed by a doctor to reduce acid production, but long-term use should be carefully monitored due to potential side effects. Working closely with a healthcare professional is essential to develop a personalized treatment plan that addresses your specific needs and minimizes risks. The link between reflux and sleep positioning can also impact symptoms significantly. Remember, persistent bloating isn’t something you simply have to live with; understanding the link between silent reflux and bloating empowers you to take control of your digestive health and find lasting relief. Also consider if GERD and sinus infections are connected in your case.