Hypermobility, often described as being “double-jointed,” is far more than just a party trick. For many, it’s an intrinsic part of their body’s structure, impacting how they move and experience the world. However, alongside increased flexibility can come a surprising array of seemingly unrelated symptoms, one of which is surprisingly common: bloating. It’s a frustrating disconnect – you might be doing everything “right” in terms of diet and lifestyle, yet consistently feel uncomfortable and swollen. Understanding why this happens for those with hypermobile joints requires looking beyond simple digestive issues and delving into the complex interplay between joint instability, nervous system regulation, and gut function. This isn’t about diagnosing a condition; it’s about exploring potential connections and empowering individuals to better understand their bodies.
The connection between hypermobility and bloating isn’t always immediately obvious, which can lead to frustration and misdiagnosis. Many people with hypermobile joints, often associated with conditions like Hypermobility Spectrum Disorder (HSD) or Ehlers-Danlos Syndrome (EDS), experience a cascade of related issues that ultimately contribute to digestive discomfort. These include proprioceptive challenges – difficulty sensing where your body is in space – leading to altered movement patterns and potentially impacting abdominal muscle function, as well as dysautonomia, a dysfunction of the autonomic nervous system which regulates many bodily functions including digestion. It’s crucial to remember that everyone experiences hypermobility differently, and the extent to which bloating is present will vary greatly. This article aims to unpack some of the key mechanisms at play, offering insights into why this symptom arises for so many with flexible joints. You might also find it helpful to understand why people with desk jobs may experience digestive issues as well.
The Interplay Between Hypermobility & Digestive Function
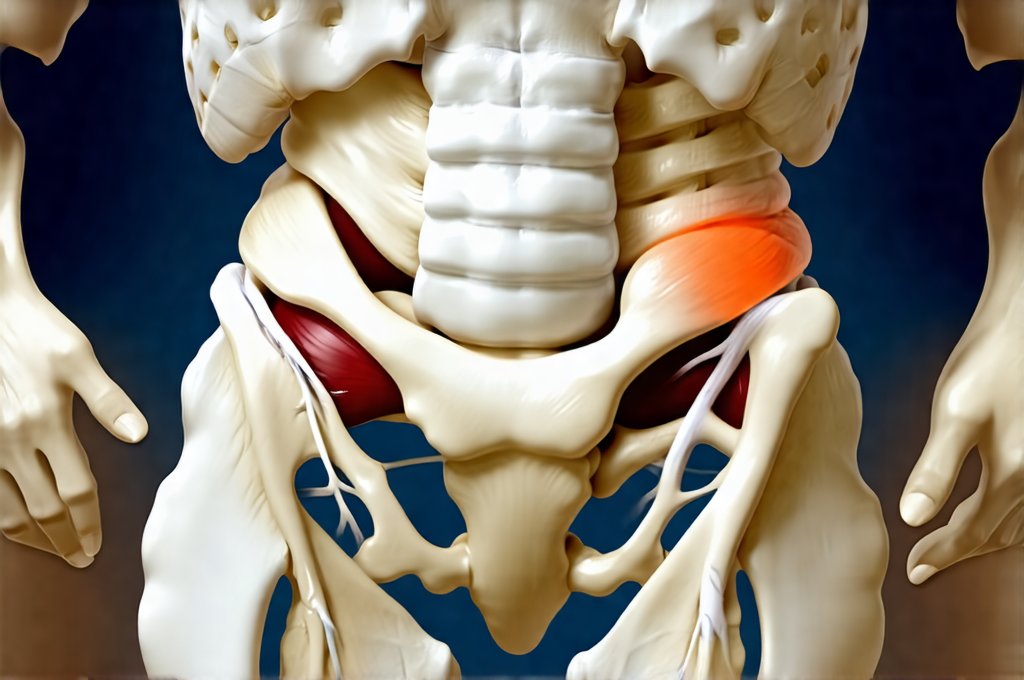
The digestive system isn’t an isolated entity; it’s deeply connected to the musculoskeletal system and nervous system. In individuals with hypermobility, several factors can disrupt optimal digestive function leading to bloating. One key aspect is altered biomechanics. Hypermobile joints often lead to compensatory movement patterns as the body tries to stabilize itself. This means that muscles work in unexpected ways, potentially affecting core stability – which plays a vital role in supporting abdominal organs and facilitating healthy digestion. – Weakened core muscles can contribute to reduced peristalsis (the wave-like muscle contractions that move food through the digestive tract), leading to constipation and subsequent bloating. – Similarly, altered posture stemming from joint instability can compress abdominal organs, hindering their function. This compression isn’t necessarily painful but can disrupt normal digestive processes. Understanding hormonal fluctuations and their impact on digestion can also be beneficial.
Beyond biomechanics, vagal nerve dysfunction is a common issue in hypermobile individuals. The vagus nerve plays a critical role in the “rest and digest” response, stimulating digestion and reducing inflammation. In those with dysautonomia – frequently co-occurring with hypermobility – vagal tone can be compromised. A weakened vagal tone means reduced digestive efficiency, slower gastric emptying (the rate at which food leaves the stomach), and increased susceptibility to bloating. This is because the gut relies on signals from the vagus nerve to coordinate its activity; without those signals, things can become sluggish and uncomfortable. Essentially, a stressed or overwhelmed nervous system prioritizes “fight or flight” over “rest and digest,” hindering optimal digestion. For some, stressful periods can significantly exacerbate these symptoms.
Finally, hypermobility itself can directly impact the tissues surrounding the digestive tract. The ligaments and connective tissues that support organs are often more lax in people with hypermobility. This lack of structural support can lead to organ prolapse (though typically mild) or increased sensitivity to stretching and movement within the abdomen, contributing to discomfort and bloating sensations. It’s a complex picture, but understanding these interconnected factors is essential for addressing the root causes of bloating in this population.
Proprioception & Abdominal Muscle Function
Proprioception – your body’s awareness of its position in space – is often impaired in individuals with hypermobility. This means they may have difficulty coordinating movements and stabilizing joints, impacting even seemingly simple actions like breathing or walking. In the context of digestion, poor proprioception can lead to inefficient abdominal muscle activation. – The transversus abdominis, a deep core muscle crucial for supporting internal organs, relies on precise neuromuscular control. If this control is compromised due to hypermobility-related proprioceptive deficits, the muscle may not fire correctly, resulting in reduced support and potential digestive issues.
Furthermore, altered movement patterns can create imbalances in abdominal pressure. When muscles aren’t working optimally, it leads to uneven tension and compression within the abdomen, hindering peristalsis and potentially causing gas buildup. This can be exacerbated by shallow breathing, which is common in those with hypermobility as they may unconsciously restrict their diaphragm due to discomfort or instability. – Restoring proprioceptive awareness through targeted exercises like Pilates or specific physiotherapy techniques can help improve abdominal muscle function and reduce bloating. These exercises focus on consciously engaging core muscles and improving body awareness. It’s also worth considering why some people get reflux without the typical heartburn symptoms, as it highlights how differently digestive issues can manifest.
The gut-brain connection also plays a significant role here. When the brain receives inaccurate information about body position (due to impaired proprioception), it can trigger stress responses that further disrupt digestive function. This creates a vicious cycle where physical instability contributes to emotional distress, which then exacerbates digestive symptoms like bloating. Addressing this requires a holistic approach that incorporates movement therapy, mindfulness practices, and potentially psychological support.
The Role of Dysautonomia & Gut Motility
Dysautonomia, or autonomic dysfunction, is highly prevalent in individuals with hypermobility. As mentioned earlier, the autonomic nervous system regulates involuntary functions like heart rate, blood pressure, digestion, and temperature control. In dysautonomia, this system doesn’t function optimally, leading to a wide range of symptoms including fatigue, dizziness, brain fog, and – crucially for our discussion – digestive issues. Specifically, gastroparesis (delayed stomach emptying) is common in those with dysautonomia. – This means food remains in the stomach for longer than it should, leading to fermentation, gas production, and ultimately, bloating.
The vagus nerve, a key component of the parasympathetic nervous system responsible for “rest and digest,” is often implicated in dysautonomia. In hypermobile individuals, vagal tone may be reduced due to chronic stress, inflammation, or direct neurological dysfunction. This diminished vagal tone slows down digestive processes, increasing susceptibility to bloating and constipation. – Conversely, some individuals with dysautonomia experience dumping syndrome, where food passes through the digestive system too quickly, leading to diarrhea and abdominal discomfort. The unpredictable nature of gut motility in dysautonomia makes it difficult to manage symptoms effectively. Understanding reflux from water can also provide insight into unexpected digestive triggers.
Managing dysautonomia requires a multifaceted approach. Hydration is paramount, as dehydration can exacerbate autonomic dysfunction. Dietary modifications – such as smaller, more frequent meals – can also help reduce the burden on the digestive system. – Other strategies include incorporating stress-reducing techniques like yoga or meditation, and working with a healthcare professional to explore potential medication options if necessary. It’s important to note that dysautonomia is often a complex condition requiring individualized treatment plans.
Inflammation & Intestinal Permeability
Chronic inflammation is increasingly recognized as a contributing factor to bloating and digestive issues in individuals with hypermobility. The laxity of connective tissues can lead to increased intestinal permeability, also known as “leaky gut.” – This occurs when the tight junctions between cells in the intestinal lining become compromised, allowing undigested food particles, toxins, and bacteria to escape into the bloodstream. This triggers an immune response, leading to systemic inflammation.
Inflammation itself can disrupt digestive function in several ways. It impairs nutrient absorption, alters gut motility, and increases sensitivity to bloating sensations. Furthermore, chronic inflammation can further weaken connective tissues, creating a vicious cycle where intestinal permeability worsens and inflammation persists. – Dietary factors play a crucial role here. Eliminating inflammatory foods like processed sugars, gluten (for those with sensitivities), and excessive dairy may help reduce inflammation and improve gut health.
Restoring gut barrier function requires a holistic approach that includes dietary modifications, stress management, and potentially supplementation with nutrients like L-glutamine or zinc. – Probiotics can also be beneficial for promoting a healthy gut microbiome, but it’s important to choose strains specifically suited to your individual needs. Addressing inflammation is not simply about symptom relief; it’s about restoring the underlying integrity of the digestive system. If you often experience discomfort, learning why you might experience a sore throat without heartburn can be helpful.
It’s vital to reiterate that this information isn’t intended as medical advice. If you are experiencing persistent bloating or other digestive symptoms, please consult with a qualified healthcare professional for personalized evaluation and treatment. They can help determine the underlying causes of your symptoms and develop a plan tailored to your specific needs.