Gas is an incredibly common digestive complaint, often dismissed as merely embarrassing, but for many, it can significantly impact quality of life. It’s not simply about social awkwardness; excessive gas frequently accompanies bloating, abdominal pain, and even changes in bowel habits, leading to discomfort that interferes with daily activities. The underlying causes are complex – ranging from dietary choices and rapid eating to stress levels and underlying gut health imbalances. While over-the-counter remedies offer temporary relief, a more sustainable approach often involves addressing the root of the problem, which frequently lies within the intricate ecosystem of our digestive system. This is where the concept of a “gut reset” diet comes into play – not as a quick fix, but as a structured process to support and restore healthy gut function, potentially alleviating troublesome gas symptoms.
A gut reset isn’t about deprivation or restrictive dieting; instead, it’s focused on strategically eliminating potential irritants, nourishing beneficial bacteria, and gradually reintroducing foods to identify individual sensitivities. It’s about understanding that the digestive system is a complex network, and what triggers gas in one person might not affect another. This approach acknowledges the bidirectional relationship between gut health and overall wellbeing – a healthy gut contributes to better digestion, nutrient absorption, immune function, and even mental health. Implementing a gut reset diet can be a proactive step towards understanding your body’s unique needs and fostering long-term digestive comfort. You might find it helpful to explore how to transition into a more gut-friendly way of eating as you begin this process.
Understanding the Gut-Gas Connection
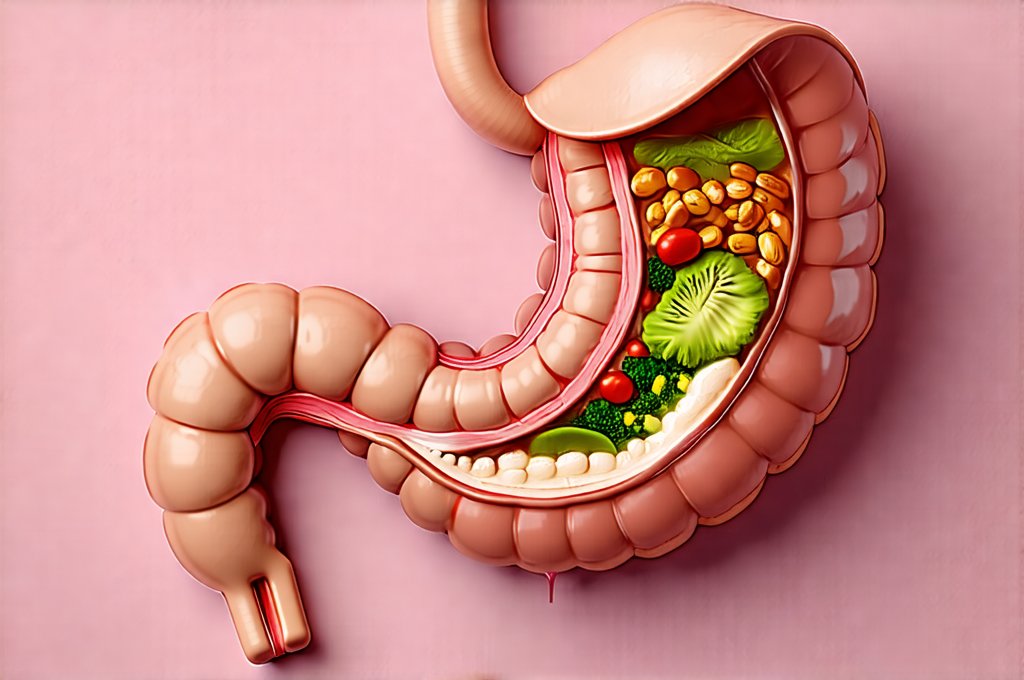
The production of gas in the digestive system is a completely normal process. It’s a byproduct of bacterial fermentation – essentially, what happens when bacteria break down undigested carbohydrates in the large intestine. However, excessive gas signals an imbalance. Several factors can contribute to this, including dietary choices high in fermentable carbohydrates (FODMAPs), rapid eating which leads to swallowing more air, and a lack of digestive enzymes. More fundamentally, imbalances within the gut microbiome – the trillions of bacteria residing in our intestines – play a critical role. An overgrowth of gas-producing bacteria or a deficiency in beneficial microbes can both lead to increased flatulence.
The composition of your gut microbiome is influenced by numerous factors: diet being paramount. A diet lacking fiber, rich in processed foods, and high in sugar can disrupt the delicate balance of bacterial populations. Stress, antibiotic use, and even chronic health conditions also impact microbial diversity. When this ecosystem is compromised, digestion becomes less efficient, leading to more undigested food reaching the large intestine and providing fuel for gas-producing bacteria. Therefore, a gut reset diet aims to address these imbalances by reducing fermentable carbohydrates, supporting beneficial bacteria growth, and improving overall digestive function. It’s also important to consider if gut symptoms might be a sign of something deeper like burnout.
A key element in managing gas symptoms through diet is identifying individual triggers. While certain foods are common culprits (beans, broccoli, onions), sensitivity varies widely. Keeping a food diary alongside the gut reset can be incredibly helpful in pinpointing which foods exacerbate your symptoms. This personalized approach ensures that dietary changes are tailored to your specific needs and avoid unnecessary restrictions. Understanding gut healing can help reduce inflammation overall, too.
The Phases of a Gut Reset Diet for Gas Relief
A typical gut reset diet unfolds in phases, each serving a distinct purpose. Phase one generally focuses on elimination – removing potential irritants like high-FODMAP foods, gluten, dairy, processed sugars, artificial sweeteners, and alcohol. This period lasts approximately 2-3 weeks, allowing the digestive system to calm down and reducing inflammation. The goal isn’t necessarily permanent elimination but rather a temporary removal to assess tolerance. Phase two is about reintroduction – systematically adding back foods one at a time, while carefully monitoring for any symptoms. This allows you to identify specific food sensitivities and understand your individual tolerance levels.
The final phase focuses on maintenance – incorporating the learnings from the previous phases into a long-term dietary strategy that supports gut health and minimizes gas production. This involves prioritizing whole, unprocessed foods, focusing on fiber-rich options (once tolerated), staying hydrated, managing stress, and continuing to listen to your body’s signals. It’s important to note this isn’t about perfection; occasional indulgences are permissible as long as they don’t significantly disrupt digestive balance. This phased approach allows for a more sustainable and personalized outcome compared to drastic dietary restrictions. If you find yourself struggling, it may be time to reset digestion with a liquid diet.
Identifying & Eliminating Trigger Foods
The elimination phase is often the most challenging, requiring discipline and awareness. Start by removing common gas-producing foods:
1. High-FODMAP foods: These include onions, garlic, apples, pears, stone fruits (peaches, plums), wheat, rye, legumes (beans, lentils), dairy products containing lactose, and certain vegetables like broccoli and cauliflower. Resources like the Monash University FODMAP diet app can be invaluable for identifying these foods.
2. Gluten: Even without celiac disease, gluten sensitivity can contribute to bloating and gas. Eliminate wheat, barley, and rye from your diet.
3. Processed Foods & Sugars: These offer minimal nutritional value and often contain additives that can disrupt gut health.
During this phase, pay close attention to how your body responds. Keep a detailed food diary, noting what you eat, when you eat it, and any associated symptoms (gas, bloating, abdominal pain). Be honest with yourself about your dietary habits and any potential triggers. This detailed record will be crucial during the reintroduction phase. Understanding gut symptoms as a warning sign can help you address issues proactively.
Reintroducing Foods Strategically
The reintroduction phase is where you regain control of your diet and identify individual sensitivities. Introduce foods one at a time, waiting 2-3 days between each new addition to monitor for symptoms. Begin with small portions and gradually increase the amount if tolerated. For example, start with a tablespoon of yogurt (if dairy was eliminated) and observe how your body reacts over the next few days. If you experience any gas, bloating, or abdominal pain, remove that food from your diet and try again later.
This process requires patience and self-awareness. It’s easy to get discouraged if you discover several sensitivities, but remember that identifying these triggers is a positive step towards improving your digestive health. Don’t be afraid to seek guidance from a registered dietitian or healthcare professional during this phase; they can provide personalized support and ensure you’re following a safe and effective reintroduction protocol. Gut healing may also improve other chronic symptoms that accompany digestive issues.
Supporting Gut Health During & After the Reset
A gut reset isn’t just about eliminating foods; it’s also about actively supporting gut health. Incorporating probiotic-rich foods into your diet, such as fermented vegetables (sauerkraut, kimchi), yogurt with live cultures (if tolerated), and kefir can help restore beneficial bacteria populations. Prebiotic foods – those that feed the good bacteria – are equally important. These include asparagus, bananas, oats, and garlic (though introduce cautiously during reintroduction).
Beyond diet, lifestyle factors play a significant role. Managing stress through techniques like meditation, yoga, or deep breathing exercises can reduce inflammation and improve digestive function. Adequate hydration is essential for optimal digestion. Finally, mindful eating – slowing down, chewing thoroughly, and paying attention to hunger cues – can significantly reduce air swallowing and improve the overall digestive process. Focusing on these aspects alongside the dietary changes will maximize the benefits of your gut reset diet and contribute to long-term digestive wellbeing. Finding a balanced gut health diet can be challenging, but ultimately very rewarding.