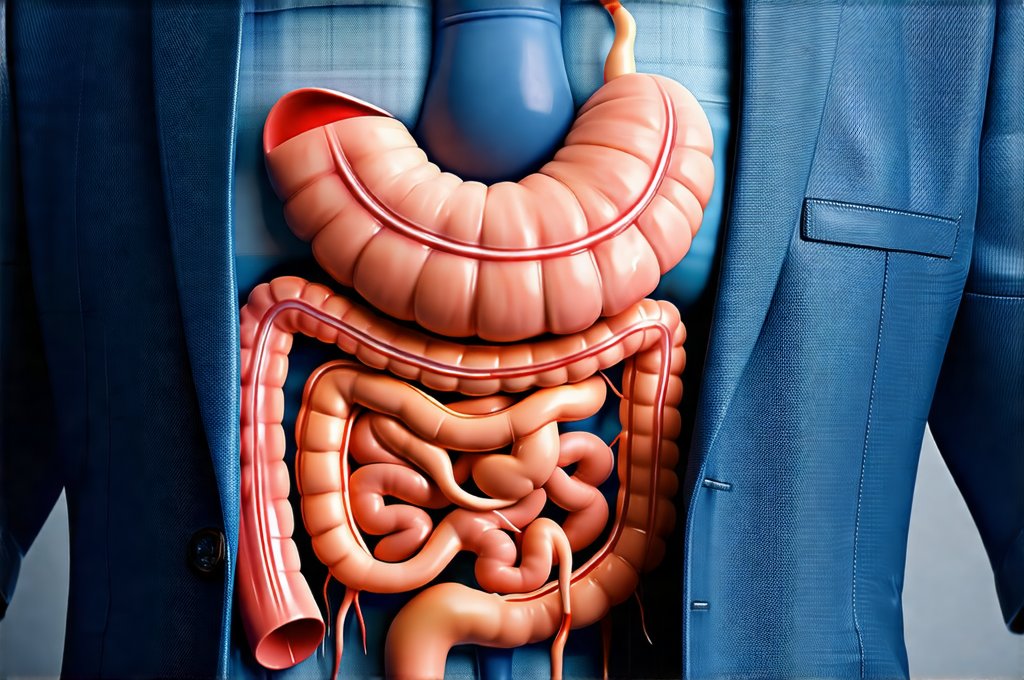
Stress is an unavoidable part of modern life, but when it becomes chronic and intense – particularly in high-pressure work environments – its effects can extend far beyond just mental and emotional wellbeing. Many people experience physical symptoms as a result of prolonged stress, and surprisingly often, these symptoms manifest in the digestive system. The gut, frequently referred to as our “second brain,” is profoundly sensitive to psychological state, making it a prime target for the physiological fallout of unmanaged stress. Understanding the intricate connection between high-stress jobs and gut health is crucial not just for managing immediate discomfort but also for preventing long-term health issues.
The relationship isn’t simply about feeling anxious and getting a stomachache; it’s a complex interplay involving hormones, neurotransmitters, the immune system, and the trillions of microorganisms that make up our gut microbiome. This bidirectional communication pathway – often called the gut-brain axis – means stress can directly impact digestive function, while imbalances in the gut can actually exacerbate feelings of anxiety and stress, creating a vicious cycle. Ignoring these connections can lead to chronic digestive problems and negatively influence overall health and quality of life. Many individuals find themselves struggling with unexplained gastrointestinal issues without realizing the root cause may lie in their work environment or stress levels. You might even wonder can gut symptoms be a sign of something deeper.
The Gut-Brain Axis: A Two-Way Street
The gut-brain axis isn’t a new concept, but recent research has dramatically illuminated its complexity. It’s not just one pathway; it’s a multifaceted communication network involving several routes. – The vagus nerve acts as a direct line of communication between the gut and the brain, transmitting signals in both directions. – The endocrine system, particularly the hypothalamic-pituitary-adrenal (HPA) axis, releases stress hormones like cortisol which significantly impact gut function. – The immune system plays a crucial role, as stress can suppress immunity, making the gut more vulnerable to inflammation and imbalances. – And importantly, the gut microbiome itself influences brain health through the production of neurotransmitters and other signaling molecules.
High-stress jobs consistently activate the HPA axis, leading to chronically elevated cortisol levels. While acute bursts of cortisol are necessary for survival – triggering fight-or-flight responses – prolonged exposure disrupts normal digestive processes. This can manifest as altered gut motility (leading to diarrhea or constipation), increased intestinal permeability (“leaky gut”), and changes in the composition of the gut microbiome. The microbiome, which is essential for digestion, nutrient absorption, and immune regulation, becomes particularly vulnerable under stress. Studies show that chronic stress can decrease microbial diversity, favoring harmful bacteria over beneficial ones. If you are struggling with this, perhaps consider can reactions be a sign of healing?
This disruption isn’t just a one-way street. An imbalanced gut microbiome can send distress signals to the brain, impacting mood, cognition, and even contributing to anxiety and depression. Certain gut bacteria produce neurotransmitters like serotonin – often called the “happy hormone” – so alterations in microbial populations can directly influence emotional wellbeing. It’s this feedback loop that makes managing stress and supporting gut health so critical for overall wellness. Addressing one without addressing the other is unlikely to yield long-term results. Understanding how your diet plays a role is key, and you may wonder can you build a tolerant gut over time?
How Stress Manifests as Gut Symptoms
The ways stress impacts the gut are incredibly varied, depending on individual sensitivity, pre-existing conditions, and the nature of the stressors themselves. One common manifestation is Irritable Bowel Syndrome (IBS). While IBS isn’t solely caused by stress, it’s significantly exacerbated by it. Stress can trigger flare-ups in individuals already diagnosed with IBS, leading to abdominal pain, bloating, gas, diarrhea, and/or constipation. The increased gut permeability associated with chronic stress can allow undigested food particles and toxins to enter the bloodstream, triggering inflammation and further exacerbating symptoms.
Beyond IBS, high stress often leads to functional dyspepsia – a condition characterized by persistent indigestion, bloating, nausea, and early satiety (feeling full quickly). This occurs because stress slows down gastric emptying, meaning food stays in the stomach longer, leading to discomfort. Stress can also contribute to heartburn and acid reflux as it increases stomach acid production and weakens the lower esophageal sphincter. Furthermore, prolonged cortisol elevation can suppress immune function in the gut, making individuals more susceptible to infections and inflammatory bowel diseases (IBD) like Crohn’s disease and ulcerative colitis – although a genetic predisposition is usually required for these conditions to develop. It’s also important to remember that how the smell of food can sometimes play a role.
Finally, it’s important to remember that stress can alter eating habits. Many people turn to comfort foods or skip meals altogether when stressed, both of which disrupt digestion and contribute to gut imbalances. Increased consumption of processed foods, sugar, and alcohol—common coping mechanisms during stressful periods—further compromises the microbiome and exacerbates digestive issues. The combination of physiological changes induced by stress and altered dietary habits creates a perfect storm for gut dysfunction. You might also wonder can gut symptoms be a warning sign?
Strategies for Mitigating Stress & Supporting Gut Health
Successfully navigating a high-stress job while protecting your gut requires a multifaceted approach that addresses both the source of the stress and the health of your digestive system. This isn’t about eliminating stress entirely—that’s often unrealistic—but rather learning to manage it effectively. Mindfulness practices, such as meditation or deep breathing exercises, can help regulate the nervous system and reduce cortisol levels. Regular physical activity is another powerful stress reliever, releasing endorphins that have mood-boosting effects. Prioritizing sleep is also paramount; aim for 7-9 hours of quality sleep each night to allow your body to recover and repair.
Dietary changes play a vital role in supporting gut health. – Incorporating prebiotic foods (like onions, garlic, bananas, asparagus) nourishes beneficial gut bacteria. – Including probiotic-rich foods (like yogurt, kefir, sauerkraut, kimchi) introduces live microorganisms that can restore microbial balance. – Reducing processed foods, sugar, and excessive alcohol intake minimizes inflammation and supports a healthy microbiome. – Consider a food sensitivity test to identify potential triggers. Taking control of your diet is important, so how to create a weekly menu that won’t trigger discomfort can be very helpful.
Beyond lifestyle changes, seeking professional support is often necessary. A therapist or counselor can provide strategies for managing stress and developing coping mechanisms. A registered dietitian can help you create a personalized nutrition plan that supports gut health. And if you suspect underlying digestive issues, consulting a gastroenterologist is essential for accurate diagnosis and appropriate treatment. Remember, taking proactive steps to manage stress and nurture your gut is an investment in your long-term wellbeing.
The Role of Workplace Culture
It’s crucial to acknowledge that individual strategies are often insufficient when the source of stress is deeply embedded within the workplace culture itself. Toxic work environments characterized by unrealistic expectations, constant pressure, lack of support, and poor communication create a breeding ground for chronic stress. Addressing these systemic issues requires organizational change. Companies need to prioritize employee wellbeing by promoting healthy work-life balance, providing access to mental health resources, fostering a supportive and collaborative environment, and recognizing the importance of boundaries.
Employees also have a role to play in advocating for their own needs and creating healthier workplace dynamics. This could involve setting clear boundaries with colleagues and managers, communicating concerns openly and assertively, and seeking support from coworkers. While it may not always be possible to change an entire company culture overnight, taking small steps towards creating a more supportive and less stressful work environment can have a significant impact on individual wellbeing.
Ultimately, the connection between high-stress jobs and gut symptoms highlights the interconnectedness of mind and body. Prioritizing both mental and physical health is essential for thriving in today’s demanding world. Understanding this relationship empowers individuals to take control of their wellbeing and advocate for healthier work environments, leading to a more balanced and fulfilling life. Also consider how GERD can mimic a heart attack.