Bloating is an incredibly common experience, impacting millions worldwide. It’s often dismissed as just “part of life,” but chronic or severe bloating can be deeply uncomfortable and significantly interfere with daily activities. The trickiest part? Identifying why you’re bloated in the first place. Many factors contribute to this sensation – from dietary choices and stress levels to underlying medical conditions. Often, bloating is categorized broadly as either digestive or lymphatic, though the lines between these systems can be surprisingly blurred. Understanding the potential source of your bloating isn’t about self-diagnosing; it’s about gaining a better understanding of your body so you can have more informed conversations with healthcare professionals and potentially explore strategies for relief.
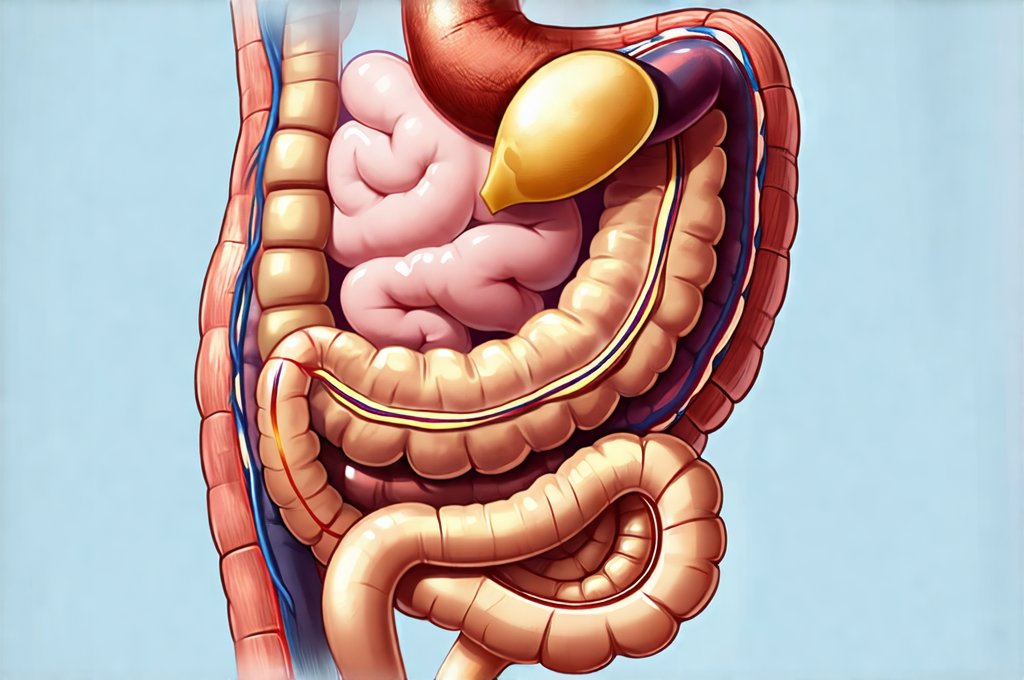
The human body is an interconnected system, meaning issues in one area often ripple outwards, impacting others. Digestive bloating stems from problems within the gastrointestinal tract – think food sensitivities, gas production, or motility issues. Lymphatic bloating, on the other hand, relates to the lymphatic system’s role in fluid balance and waste removal. This system can become congested, leading to swelling that feels different than typical digestive discomfort. Discerning these differences requires careful observation of your symptoms, timing, and associated factors. It’s crucial to remember that this is about understanding potential causes; only a medical professional can provide an accurate diagnosis and personalized treatment plan. Consider exploring how to decode your body’s signals for more insight.
Recognizing Digestive Bloating
Digestive bloating is arguably the more commonly recognized type. It’s directly tied to what we eat and how our bodies process it. The sensation typically feels localized around the abdomen, often accompanied by gas, cramping, or changes in bowel habits. A key characteristic is its direct correlation with meals. You might notice bloating shortly after eating, especially certain foods that are known triggers for many people. These can include: – High-FODMAP foods (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) – found in onions, garlic, apples, wheat, dairy etc. – Carbonated beverages – Artificial sweeteners – Fatty or fried foods – Legumes and cruciferous vegetables (broccoli, cauliflower)
The timing of digestive bloating is also important. It often follows a predictable pattern based on your eating schedule. For instance, if you consistently experience bloating after breakfast, it could point to an issue with something in your morning meal. Furthermore, digestive bloating frequently responds well to dietary adjustments and over-the-counter remedies designed to aid digestion – things like enzyme supplements or peppermint tea. However, persistent digestive bloating warrants medical attention, as it could indicate underlying conditions such as irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), or food intolerances/allergies. If you’re unsure is it GERD or something else?
Digestive discomfort can manifest in various ways beyond simple bloating. Diarrhea, constipation, heartburn, and nausea are all common accompanying symptoms. Paying attention to these associated symptoms helps paint a more complete picture. Consider keeping a food diary for a week or two, meticulously recording what you eat, when you eat it, and any digestive symptoms that follow. This can help identify potential trigger foods or patterns. Remember, even seemingly harmless foods can cause issues for some individuals; everyone’s digestive system is unique. You might also want to check if you’re reacting to spices.
Identifying Lymphatic Bloating
Lymphatic bloating is often more subtle and pervasive than its digestive counterpart. It’s less about immediate post-meal discomfort and more about a general feeling of swelling, particularly in the extremities (arms, legs, ankles) but also potentially around the abdomen or face. Unlike digestive bloating which tends to fluctuate rapidly with meals, lymphatic congestion develops more gradually. The sensation is often described as a heavy, achy fullness rather than sharp cramping or gas pains. It’s important to note that lymphatic swelling isn’t always confined to the abdominal area; it can impact various parts of the body depending on where lymph flow is restricted.
The lymphatic system plays a vital role in removing waste and toxins from the body. When this system becomes overloaded – due to factors like dehydration, lack of exercise, stress, or certain medical conditions – fluid accumulates, leading to swelling. This isn’t necessarily about excess water intake; it’s about the lymphatic system’s inability to effectively move fluids. Unlike digestive bloating which is often relieved by dietary changes, lymphatic bloating may require strategies that support lymphatic drainage. These include: – Regular gentle exercise (walking, yoga) – Deep breathing exercises – Lymphatic massage – Staying adequately hydrated
A key distinguishing feature of lymphatic bloating is its potential association with other symptoms related to immune function. Frequent illness, fatigue, skin rashes, and even brain fog can all be indicators of a compromised lymphatic system. While digestive issues are less common as direct accompaniments, you might experience subtle digestive changes due to the overall impact of lymphatic congestion on bodily functions. If you suspect lymphatic bloating, it’s crucial to rule out more serious medical conditions that could mimic these symptoms, such as kidney problems or heart failure. Understanding what your stomach is telling you can provide clues.
When to Seek Professional Help
Determining whether your bloating is primarily digestive or lymphatic shouldn’t be a substitute for professional medical evaluation. If your bloating is severe, persistent, or accompanied by concerning symptoms like significant weight loss, blood in the stool, fever, or intense pain, seek immediate medical attention. These could indicate underlying health issues that require prompt diagnosis and treatment. Even if your symptoms are milder, it’s wise to consult a healthcare professional if they interfere with your quality of life.
A doctor can perform various tests to help pinpoint the cause of your bloating. These might include: – Blood tests to check for inflammation or infections – Stool tests to identify gut imbalances – Food allergy/intolerance testing – Imaging scans (X-rays, CT scans) to visualize the digestive system – and in some cases, lymphatic structures – Lymphatic drainage assessment
Remember, self-diagnosis can be misleading. A healthcare professional can provide an accurate diagnosis and develop a personalized treatment plan based on your individual needs. This might involve dietary changes, medication, lifestyle modifications, or referral to a specialist (such as a gastroenterologist or lymphedema therapist). Don’t hesitate to advocate for yourself and seek the support you need to address your bloating effectively. Consider how to travel without triggering symptoms if you have plans. It’s also beneficial to explore how to know if your gut is healing, and finally, if your reflux is acidic. Ultimately, understanding the potential origins of your discomfort is the first step towards reclaiming control of your well-being.