Reflux, often experienced as heartburn or acid indigestion, is something many people brush off as an occasional discomfort. It’s easy to dismiss – a spicy meal, a late-night snack, stress – these are all common culprits we readily identify and attribute the sensation to. We might reach for over-the-counter remedies, adjust our diets temporarily, or simply hope it goes away on its own. However, consistently ignoring persistent reflux symptoms can lead to a cascade of increasingly serious health problems that extend far beyond occasional discomfort. It’s not merely an inconvenience; untreated reflux can silently erode your quality of life and even threaten long-term health.
The human body is remarkably resilient, often compensating for minor imbalances without noticeable consequences. But chronic irritation, like that caused by frequent acid exposure, eventually overwhelms these natural defenses. What begins as a bothersome burning sensation in the chest can gradually evolve into more severe conditions impacting the esophagus, respiratory system, and even dental health. Understanding the potential ramifications of prolonged, unaddressed reflux is crucial for proactive healthcare and preventing significant complications down the line. This isn’t about inducing anxiety; it’s about empowering you with knowledge to recognize when reflux requires professional attention. Are you eating too late for good digestion?
The Escalating Consequences of Untreated Reflux
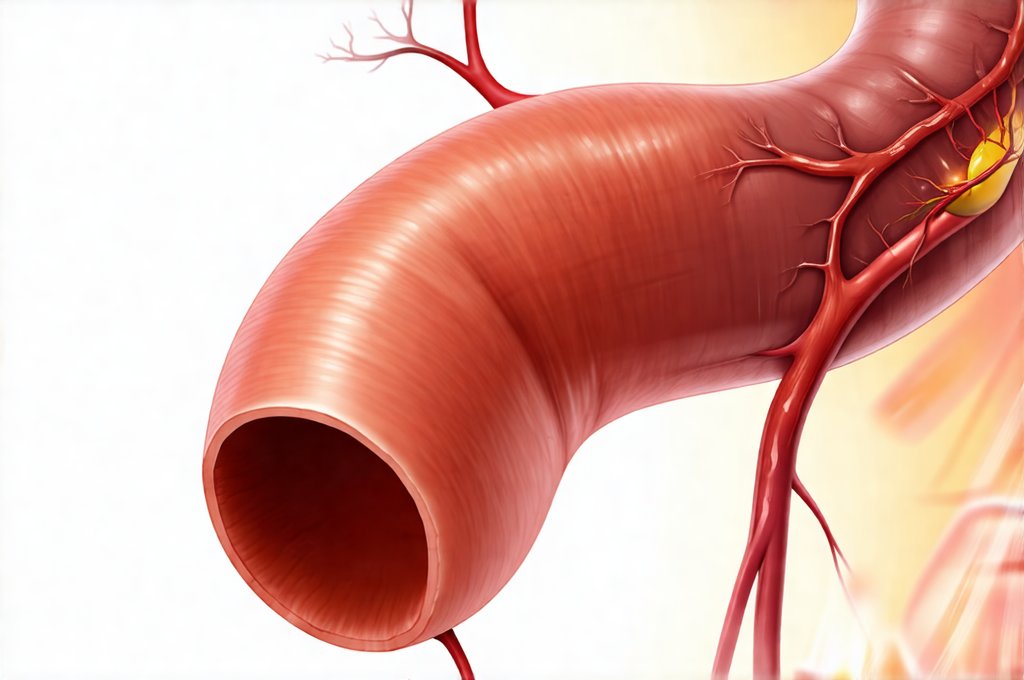
Ignoring reflux symptoms isn’t like ignoring a fleeting headache. It’s allowing a chronic condition to progress, potentially leading to significant and sometimes irreversible damage. The initial discomfort is usually caused by stomach acid flowing back up into the esophagus – this is gastroesophageal reflux. Over time, this repeated exposure can wear away at the delicate lining of the esophagus, creating inflammation and eventually causing more serious complications. One of the most common outcomes is erosive esophagitis, where the esophageal lining becomes inflamed and ulcers form. These ulcers aren’t just painful; they impede normal swallowing and can lead to bleeding.
Beyond the esophagus itself, untreated reflux can have far-reaching effects. The airway can be affected by ‘refluxed’ stomach acid, leading to chronic coughs, asthma exacerbations, or even pneumonia. This is because the acidic material can irritate the lungs and trigger inflammatory responses. Furthermore, the constant exposure to acid can damage tooth enamel, increasing the risk of cavities and dental erosion. It’s a systemic issue; reflux isn’t confined to just one part of the digestive system. The progression often happens gradually, making it easy to normalize symptoms or attribute them to other causes. What starts as occasional heartburn might evolve into daily discomfort, difficulty swallowing, a persistent cough, or even voice changes. This insidious nature is why early diagnosis and intervention are so important – preventing escalation requires recognizing the warning signs and seeking medical evaluation before irreversible damage occurs. Ignoring reflux isn’t just ignoring discomfort; it’s potentially ignoring serious health risks. Are you mistaking hunger for reaction?
Complications: Barrett’s Esophagus & Beyond
One of the most concerning long-term complications of chronic, untreated reflux is Barrett’s esophagus. This condition develops when the normal cells lining the esophagus are replaced by cells similar to those found in the intestine. It’s a direct result of prolonged acid exposure and represents a significant change in esophageal tissue. While many people with Barrett’s esophagus never develop further complications, it dramatically increases the risk of adenocarcinoma, a type of esophageal cancer.
- The development of Barrett’s esophagus is often asymptomatic, meaning you might not know you have it until routine screening or investigations for other reflux symptoms reveal its presence.
- Regular endoscopic surveillance (examination of the esophagus with a camera) is crucial for individuals diagnosed with Barrett’s esophagus to monitor for any cellular changes that could indicate cancer development.
- Lifestyle modifications and medications aimed at reducing acid exposure can help manage Barrett’s esophagus and potentially slow or even reverse some tissue changes, although this isn’t always possible.
The link between Barrett’s esophagus and esophageal cancer is a serious one, highlighting the importance of proactive management of reflux symptoms. Early detection through screening and appropriate intervention are key to improving outcomes if cancer develops. It’s also important to note that the risk of developing adenocarcinoma is relatively low in individuals with Barrett’s Esophagus, but it’s significantly higher than in those without the condition. What happens when you eat foods you’re sensitive to?
Respiratory Issues Linked to Reflux
Many people don’t associate reflux with respiratory problems, yet the connection is surprisingly common and significant. Laryngopharyngeal reflux (LPR), often referred to as “silent reflux” because it doesn’t always present with typical heartburn symptoms, can have a profound impact on the upper airway. In LPR, stomach acid reaches the larynx (voice box) and pharynx (throat), causing inflammation and irritation. This can lead to a variety of respiratory symptoms that are often misdiagnosed as allergies or asthma.
One common symptom is chronic cough, particularly at night when lying down increases the likelihood of reflux. Hoarseness, sore throat, difficulty swallowing, and a sensation of a lump in the back of the throat (globus sensation) are also frequently reported. In some cases, LPR can trigger or exacerbate asthma symptoms, making breathing more difficult. The constant irritation from acid exposure inflames the airways, leading to increased sensitivity and reactivity.
Addressing reflux through lifestyle changes and medication can often significantly improve respiratory symptoms associated with LPR. This might involve dietary modifications (avoiding trigger foods), elevating the head of the bed during sleep, and taking medications to reduce stomach acid production. The key is recognizing that the respiratory issues may be linked to reflux rather than a primary lung condition. Are you drinking too much for your gut?
Dental Erosion & Oral Health Concerns
The impact of reflux extends beyond the digestive and respiratory systems; it can also significantly affect oral health. Stomach acid is highly corrosive, and when it frequently flows back up into the mouth, it erodes tooth enamel – the protective outer layer of teeth. This erosion weakens teeth, making them more susceptible to cavities, sensitivity, and even structural damage.
- Acid erosion isn’t always obvious at first; it can be subtle and gradual, leading to changes in tooth shape and color over time.
- Individuals with reflux may experience increased tooth sensitivity to hot or cold temperatures, as the underlying dentin (tooth structure beneath enamel) becomes exposed.
- Regular dental checkups are crucial for detecting early signs of acid erosion and implementing preventative measures.
Preventative strategies include practicing good oral hygiene, using fluoride toothpaste, and potentially incorporating saliva-stimulating products into your routine. Some dentists may also recommend applying a protective coating to the teeth to help shield them from acid exposure. Furthermore, managing reflux itself through lifestyle changes or medication is essential for minimizing the impact on dental health. Protecting your teeth requires addressing the underlying reflux issue. What happens if you ignore food sensitivities?
Ultimately, ignoring reflux symptoms isn’t a passive act; it’s a decision with potentially far-reaching consequences. While occasional heartburn is usually nothing to worry about, persistent or worsening symptoms should prompt medical evaluation. Early diagnosis and intervention can prevent serious complications like Barrett’s esophagus, respiratory problems, and dental erosion, ultimately preserving your health and quality of life. Remember, proactive healthcare isn’t just about treating illness; it’s about preventing it. Are you eating too clean for your gut? What to do if you react to supplements?