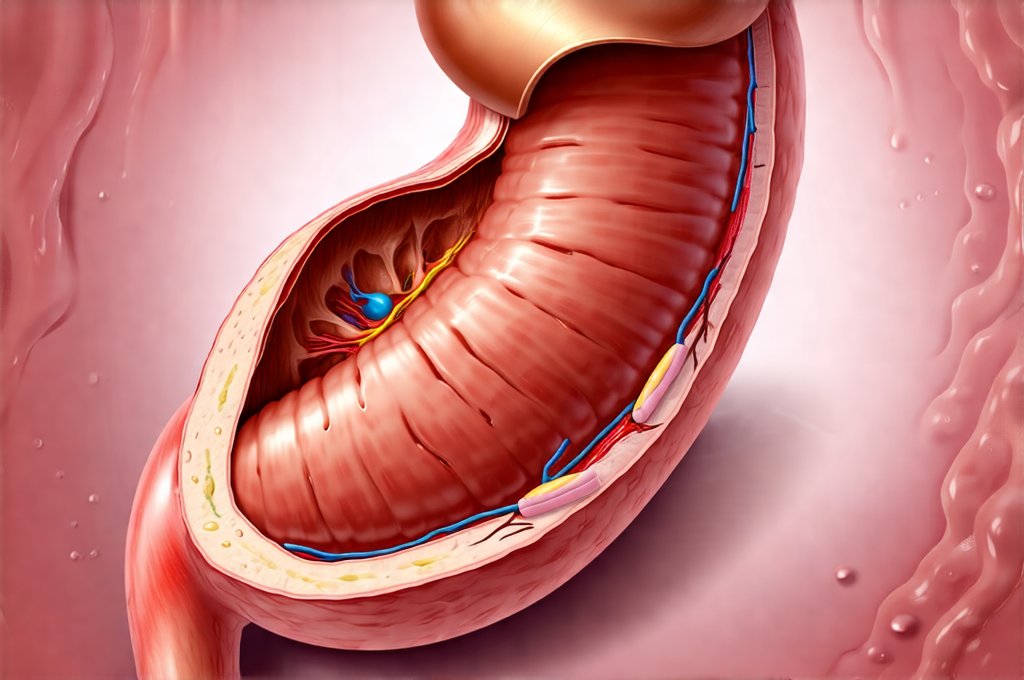
The human digestive system is a remarkable feat of biological engineering, designed to efficiently process nutrients from food while protecting vulnerable areas like the esophagus from damage. A critical component in this protective mechanism is the lower esophageal sphincter (LES), a muscular ring that acts as a valve between the stomach and the esophagus. This valve’s proper function is essential for preventing acid reflux, where stomach contents, including harsh digestive acids, flow back up into the esophagus. Overeating, a common habit in many cultures and increasingly prevalent due to readily available food options, can significantly impact the LES and its ability to perform this vital role, often leading to uncomfortable symptoms and potentially more serious health concerns over time.
While occasional indulgence is generally harmless, chronically exceeding the stomach’s capacity places undue stress on the entire digestive system. This isn’t simply about consuming too much food; it’s also related to the type of food, eating speed, and individual physiological factors. Overeating doesn’t necessarily cause immediate, dramatic failure of the LES in most people, but rather a gradual weakening or alteration of its function over extended periods. This can manifest as increased frequency and severity of heartburn, indigestion, and other gastrointestinal issues. Understanding how this occurs is key to making informed lifestyle choices that support digestive health and minimize potential complications. Recognizing the connection between anxiety can also help you understand your symptoms, as stress often exacerbates digestive issues.
The Lower Esophageal Sphincter & Its Vulnerabilities
The LES isn’t a static structure; it operates based on intricate neurological and physiological mechanisms. It remains contracted most of the time, preventing reflux, but relaxes during swallowing to allow food to pass into the stomach. This relaxation is carefully coordinated with each swallow, ensuring that only food moves downward and not upward. Several factors contribute to maintaining LES tone and proper function:
- Intrinsic muscle strength: The inherent ability of the sphincter muscles to contract and stay closed.
- Hormonal influences: Certain hormones can affect LES tone; for example, some promote relaxation while others enhance contraction. Understanding hormones and stomach pain is vital to overall digestive health.
- Pressure gradients: The natural pressure difference between the esophagus and stomach helps keep the valve closed. A significantly increased pressure in the stomach due to overeating can overwhelm this gradient.
- Nervous system control: Neural pathways regulate LES function and coordinate its activity with swallowing.
Overeating directly impacts several of these factors, primarily by increasing intragastric pressure – the pressure within the stomach. When the stomach is overly full, it stretches considerably. This stretching not only puts physical strain on the LES but can also disrupt the normal neurological signals that control it. Repeated episodes of overfilling contribute to a gradual weakening and loss of responsiveness in the sphincter. It’s akin to repeatedly stretching a rubber band; eventually, it loses its elasticity. Furthermore, certain foods exacerbate this issue. High-fat meals, for instance, take longer to digest, leading to prolonged stomach distension and increased pressure on the LES.
The relationship is often cyclical: overeating leads to increased acid reflux, which can further irritate the esophagus and potentially contribute to a weakened or damaged LES over time. This creates a feedback loop that makes symptoms worse and harder to manage. It’s important to note that individual susceptibility varies significantly; some people are naturally more prone to reflux than others due to anatomical differences or underlying conditions. However, even individuals with relatively strong LES function can experience problems if they consistently overeat. How GERD affects your throat and voice is also important to consider when experiencing these symptoms.
Consequences Beyond Heartburn: Long-Term Effects & Complications
While heartburn is the most common symptom associated with a compromised LES caused by overeating, the long-term consequences can be far more serious. Chronic acid reflux, known as gastroesophageal reflux disease (GERD), isn’t just uncomfortable; it can lead to significant health problems. One major concern is esophagitis, inflammation of the esophageal lining due to repeated exposure to stomach acid. Over time, this inflammation can cause scarring and narrowing of the esophagus, making swallowing difficult – a condition called stricture.
Another serious complication is Barrett’s esophagus. This occurs when the cells lining the esophagus change in response to chronic acid exposure. These altered cells resemble those found in the intestine and are considered precancerous. While not everyone with Barrett’s esophagus develops cancer, it significantly increases the risk of esophageal adenocarcinoma, a relatively rare but aggressive type of cancer. The connection between overeating, GERD, Barrett’s esophagus, and esophageal cancer underscores the importance of addressing this issue proactively. Understanding the link between ulcers and stomach cancer can provide further insight into long term complications.
Beyond these direct effects on the esophagus, chronic acid reflux can also impact other areas:
- Respiratory problems: Acid reflux can sometimes travel up into the airway, causing asthma symptoms or even pneumonia.
- Dental erosion: Stomach acid can erode tooth enamel, leading to cavities and sensitivity.
- Chronic cough: Reflux can trigger a persistent cough reflex.
Modifying Eating Habits for LES Health
Addressing overeating isn’t about strict dieting; it’s about cultivating mindful eating habits that respect the digestive system’s capacity. Here are several strategies:
- Portion Control: Reduce portion sizes gradually. Using smaller plates and bowls can visually cue you to eat less. Pay attention to serving size recommendations on food packaging, but remember these are often generous estimates.
- Eating Speed: Slow down your eating pace. It takes approximately 20 minutes for the brain to register fullness signals from the stomach. Eating quickly bypasses these signals, leading to overconsumption. Chew your food thoroughly and savor each bite.
- Mindful Eating: Eliminate distractions during meals—turn off the TV, put away your phone, and focus on your food. Pay attention to hunger and fullness cues. Ask yourself if you’re truly hungry or eating out of boredom, stress, or habit.
Beyond these behavioral changes, dietary adjustments can also play a crucial role. Avoiding trigger foods that exacerbate reflux – such as fatty foods, chocolate, caffeine, alcohol, and spicy foods – can help reduce pressure on the LES and minimize irritation. Eating smaller, more frequent meals throughout the day instead of large, infrequent ones can also help prevent excessive stomach distension. It’s helpful to know how to differentiate between allergy and intolerance when making dietary changes.
The Role of Body Position & Timing
The position of your body, particularly after eating, significantly impacts how well the LES functions. Gravity assists in keeping stomach contents down when you’re upright. Lying down soon after a meal allows stomach acid to flow more easily into the esophagus. It’s generally recommended to wait at least two to three hours after eating before lying down or going to bed.
- Elevating the head of your bed: Raising the head end of your bed by 6-8 inches can help prevent nighttime reflux. This isn’t simply about using extra pillows, which doesn’t provide consistent support.
- Avoiding tight clothing: Tight belts and clothing around the abdomen can increase intragastric pressure.
- Timing Meals: Adjust meal times to avoid eating large meals close to bedtime.
When to Seek Professional Help
While lifestyle modifications often alleviate symptoms associated with a weakened LES, it’s crucial to seek medical attention if problems persist or worsen. Persistent heartburn that doesn’t respond to over-the-counter medications could indicate GERD or other underlying conditions. A healthcare professional can diagnose the issue accurately and recommend appropriate treatment options.
- Medications: Proton pump inhibitors (PPIs) and H2 receptor antagonists can reduce stomach acid production, providing relief from symptoms.
- Diagnostic Tests: Endoscopy allows a visual examination of the esophagus and stomach to identify inflammation or other abnormalities. Esophageal manometry measures the pressure within the esophagus and assesses LES function.
- Surgery: In rare cases, surgery may be necessary to strengthen the LES or prevent reflux.
It’s important to remember that self-treating can mask underlying problems and delay proper diagnosis. If you suspect your overeating is contributing to digestive issues, consulting a doctor is the best course of action for personalized guidance and care. Focusing on mindful eating, making appropriate dietary changes, and addressing any underlying health concerns are all crucial steps towards protecting your esophageal valve and maintaining long-term digestive health. Understanding the connection between GERD and throat clearing can provide additional context when seeking professional help. Also, consider gut pain and additives.