Gastroesophageal reflux disease (GERD), commonly known as acid reflux, affects millions worldwide. Most people experience occasional heartburn – that burning sensation in the chest after a large meal – and manage it with over-the-counter remedies or lifestyle adjustments. However, when reflux becomes frequent, severe, or accompanied by unusual symptoms, it signals something more than just an irritating inconvenience. It can indicate your reflux is spiraling out of control, potentially leading to long-term health complications if left unaddressed. Recognizing these less obvious signs is crucial for proactive management and seeking appropriate medical evaluation.
Many associate acid reflux solely with heartburn, but the reality is far more complex. The digestive system is interconnected, and when it’s disrupted by persistent reflux, symptoms can manifest in surprising ways throughout the body. These aren’t simply “alternative” presentations of GERD; they are indicators that the ongoing inflammation and irritation caused by uncontrolled reflux are impacting other systems – from your respiratory health to your dental well-being, and even your sleep patterns. Understanding these atypical signs isn’t about self-diagnosing but rather being informed enough to advocate for your own health and seek professional guidance when necessary. This article will delve into the unexpected ways uncontrolled reflux can reveal itself, empowering you to recognize potential issues early on.
Beyond Heartburn: Recognizing Atypical Reflux Symptoms
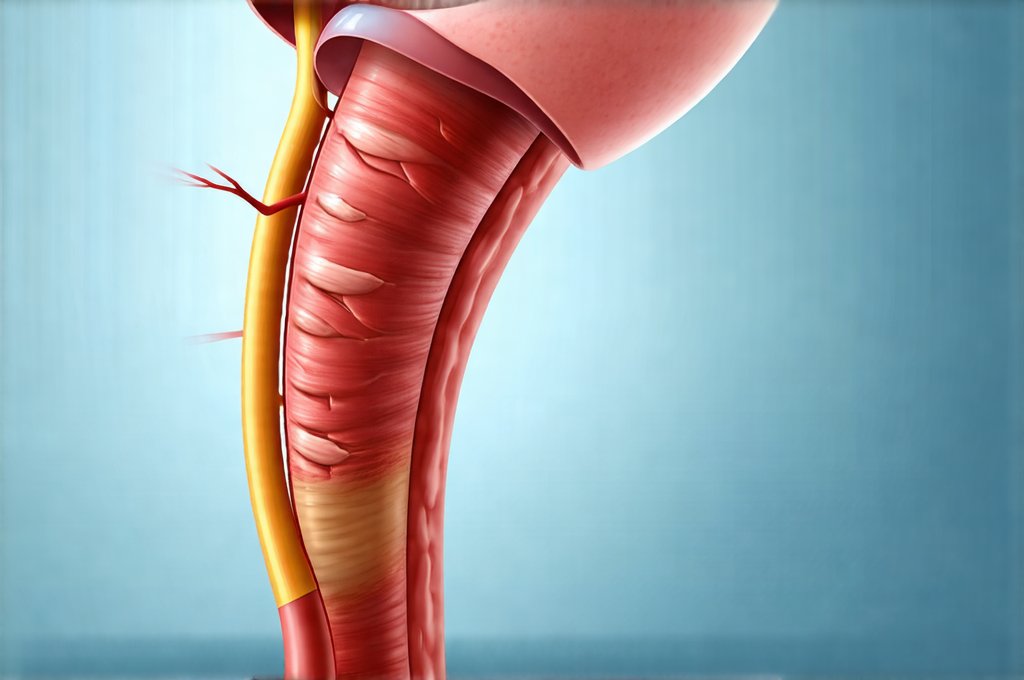
While heartburn remains the hallmark symptom of GERD, focusing solely on it can lead to delayed diagnosis and treatment if more subtle signs are present. Atypical symptoms often masquerade as other conditions, making them easily overlooked or dismissed. One common presentation is respiratory issues. Chronic acid reflux can cause micro-aspiration – tiny amounts of stomach acid entering the lungs – leading to persistent coughing, especially at night, wheezing, and even a chronic sore throat that doesn’t respond to typical treatments. This isn’t necessarily an allergy or cold; it could be your reflux irritating your airways.
Another often-missed sign is dental erosion. Stomach acid, when frequently regurgitated, can slowly dissolve tooth enamel, leading to increased sensitivity, cavities, and a general deterioration of oral health. You might notice your teeth becoming more sensitive to hot or cold temperatures, or that you’re needing more frequent dental work. Furthermore, unexplained hoarseness or a feeling like something is constantly stuck in your throat (globus sensation) can also be linked to reflux. The acid irritates the vocal cords and esophageal lining, causing these discomforting sensations.
It’s important to remember that experiencing one or two of these symptoms doesn’t automatically mean you have uncontrolled reflux. However, if you experience a cluster of these atypical manifestations alongside occasional heartburn, or even without any noticeable heartburn at all, it warrants further investigation with your healthcare provider. Many individuals with “silent reflux” – reflux without typical heartburn – can still experience significant damage to the esophagus and other organs due to ongoing acid exposure. If you suspect early signs of gut imbalance, it’s best to get checked out promptly.
The Sleep Disruption Connection
Uncontrolled reflux frequently disrupts sleep in several ways, creating a vicious cycle where poor sleep exacerbates reflux symptoms, and vice versa. – Difficulty falling asleep or staying asleep are common complaints among individuals with GERD. Lying flat can worsen reflux, leading to nighttime heartburn that keeps you awake. – Nighttime coughing or choking sensations due to micro-aspiration also severely disrupt sleep quality. – Even if you don’t consciously experience heartburn, the discomfort from silent reflux can trigger arousal from sleep without you fully realizing why.
This chronic sleep deprivation has far-reaching consequences beyond just feeling tired. It weakens your immune system, increases stress levels, and makes it harder to manage other health conditions. Moreover, disrupted sleep often leads to increased fatigue during the day, impacting productivity and overall quality of life. If you consistently wake up feeling unrested despite getting adequate hours in bed, or if you experience frequent nighttime awakenings accompanied by respiratory symptoms, consider exploring the possibility that uncontrolled reflux is a contributing factor. Understanding how to eat out without stressing your gut can also help minimize these disruptions.
The Impact on Mental Wellbeing
The chronic discomfort and disruption to daily life caused by uncontrolled reflux can significantly impact mental wellbeing. Persistent physical symptoms often lead to increased anxiety and stress, creating a negative feedback loop where stress further exacerbates reflux symptoms. Individuals may find themselves constantly worrying about triggering foods or situations, leading to social isolation and limitations in their activities. – Chronic pain associated with reflux can contribute to feelings of depression and hopelessness. – The frustration of managing a persistent condition that doesn’t seem to improve can also take a toll on mental health.
It’s vital to recognize the link between physical and mental health when dealing with uncontrolled reflux. Seeking support from a therapist or counselor alongside medical treatment can be immensely beneficial in coping with the emotional challenges of living with a chronic condition. Ignoring these psychological effects can lead to a worsening of both the physical symptoms and overall quality of life. If your child is experiencing discomfort, remember when belly pain is your child’s way of saying help.
Recognizing Red Flags: When To Seek Immediate Medical Attention
While many reflux symptoms can be managed with lifestyle changes and over-the-counter medications, certain red flags indicate a potentially serious situation requiring immediate medical attention. – Difficulty swallowing (dysphagia) – feeling like food is stuck in your throat or esophagus – could signify esophageal stricture or other complications. – Unintentional weight loss accompanied by reflux symptoms may suggest a more severe underlying condition. – Severe chest pain that mimics a heart attack requires urgent evaluation to rule out cardiac issues, even if you know you have reflux.
- Persistent vomiting or black, tarry stools are signs of gastrointestinal bleeding and necessitate immediate medical intervention. These aren’t typical reflux symptoms; they indicate something is seriously wrong within the digestive system. Don’t hesitate to seek emergency care if you experience any of these red flags. It’s important to be aware of warning signs of gut damage and address them quickly. Additionally, recognizing signs of silent reflux in babies is crucial for infants. And to support overall gut health, consider understanding signs of poor diet for your gut. Finally, know how to know if your gut is healing to track progress and maintain long-term wellness.
It’s crucial to remember that this information is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always consult with your physician or other qualified healthcare provider with any questions you may have regarding a medical condition.