Gastroesophageal reflux disease (GERD) is often understood as a digestive issue – heartburn, acid indigestion, those uncomfortable sensations after eating. But increasingly, healthcare professionals are recognizing the complex interplay between physical symptoms and psychological factors, particularly stress and anxiety. What many people don’t realize is that seemingly unrelated habits, like jaw clenching (also known as bruxism), can significantly contribute to GERD symptoms, creating a frustrating cycle where physical tension exacerbates digestive issues, which in turn heightens stress, leading to more tension – a true stress-reflux loop. Understanding this connection isn’t about blaming anyone for their condition; it’s about empowering individuals with knowledge and potential strategies for managing both the physical and emotional components of GERD.
This article delves into the often overlooked relationship between GERD and jaw clenching, exploring how these two conditions can feed off each other. We will examine the physiological mechanisms linking them, the role of stress in this dynamic, and practical approaches to break the cycle. It’s important to note that while this information is intended to be informative, it does not constitute medical advice. If you suspect you have GERD or bruxism, please consult with a qualified healthcare professional for diagnosis and personalized treatment recommendations. The goal here is to provide clarity on a nuanced issue and offer potential avenues for discussion with your doctor.
The Physiological Link: How Jaw Clenching Impacts Digestion
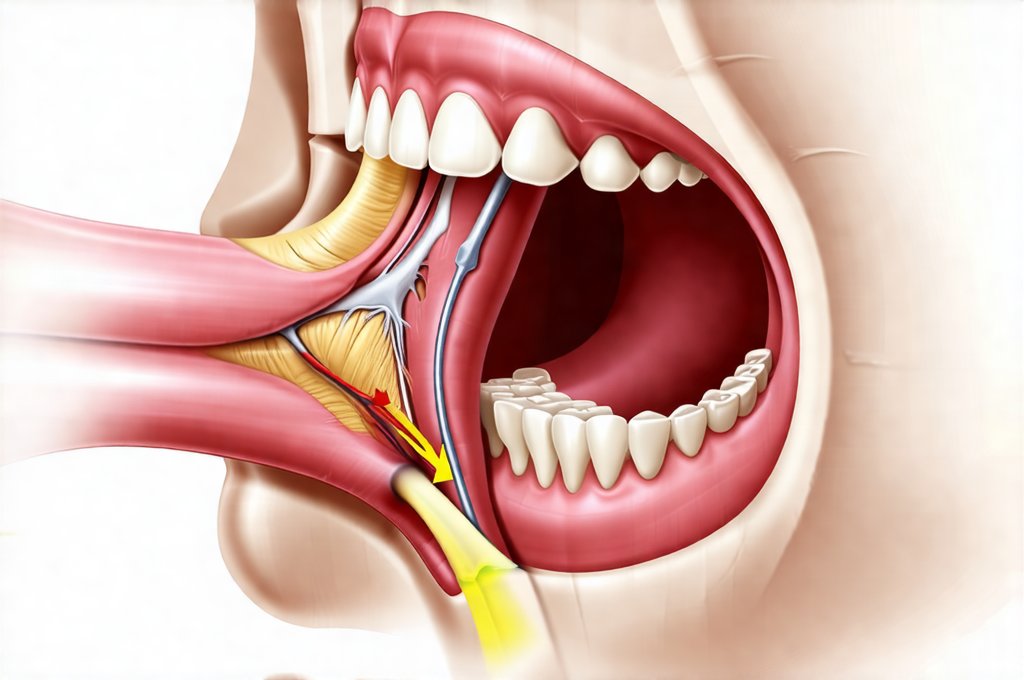
The connection between jaw clenching and GERD isn’t immediately obvious, but it stems from the intricate relationship between the muscles of the head, neck, and digestive system. Jaw clenching, even subconscious clenching during sleep, dramatically increases muscle tension in the temporomandibular joint (TMJ) – the joint connecting your jaw to your skull. This tension doesn’t stay localized; it radiates outwards, impacting surrounding muscles including those in the neck and shoulders. These connected muscular imbalances can directly affect esophageal function and contribute to GERD symptoms.
Specifically, increased muscle tension around the esophagus can disrupt normal peristalsis – the wave-like contractions that move food down into your stomach. This disruption can lead to delayed gastric emptying (food staying in the stomach longer), increasing pressure within the abdomen and potentially forcing stomach acid back up into the esophagus. Furthermore, chronic jaw clenching can alter posture, leading to a forward head position which compresses the abdominal cavity, further exacerbating reflux. It’s not simply about where you’re tense; it’s about how that tension affects overall body mechanics and digestive processes.
Beyond direct esophageal impact, jaw clenching often goes hand-in-hand with increased stress hormones like cortisol. Cortisol, while essential for survival in acute situations, chronically elevated levels can disrupt the entire digestive process – reducing stomach acid production (ironically sometimes worsening GERD long-term through impaired food breakdown), slowing down gut motility and increasing visceral hypersensitivity (meaning you perceive normal digestive sensations as painful). This creates a feedback loop: clenching leads to stress hormones, which worsen digestion, leading to more reflux, which increases stress, and so on. The role of stress in acid reflux is significant in these cases.
Stress, Anxiety, and the Reflux-Clench Cycle
Stress is arguably the central conductor in this orchestra of symptoms. It’s well-established that stress significantly worsens GERD for several reasons. Physiologically, as mentioned above, stress elevates cortisol levels. Psychologically, stress can lead to changes in eating habits – hurried meals, overeating, consuming trigger foods – all of which contribute to reflux. But the connection goes deeper than just immediate reactions to stress. Many individuals with chronic GERD experience heightened anxiety about their symptoms themselves, creating a cycle of anticipatory fear and hypervigilance.
This anticipation leads to increased muscle tension throughout the body, including in the jaw. It’s a common coping mechanism: unconsciously clenching your teeth as a way to physically “hold things together” when feeling overwhelmed or anxious. This subconscious habit can become deeply ingrained, even outside of acutely stressful situations. The brain associates certain stressors (or even just the thought of potential stressors) with jaw clenching, perpetuating the cycle. Acid reflux and anxiety often go hand in hand. Consider these points:
- Individuals prone to anxiety often exhibit higher rates of bruxism.
- The act of clenching can provide a temporary sense of control during stressful moments.
- Chronic stress desensitizes individuals to their own tension, making it harder to recognize and address jaw clenching.
Breaking this cycle requires addressing both the physical symptoms (GERD and bruxism) and the underlying emotional drivers (stress and anxiety). Ignoring one aspect will likely result in limited long-term success. It’s about recognizing that your body is communicating stress in multiple ways, and responding with holistic care. Understanding the impact of stress can help manage these conditions.
Strategies for Breaking the Loop: A Multifaceted Approach
Addressing this interplay between GERD and jaw clenching requires a multifaceted approach, combining lifestyle modifications, physical therapies, and potentially psychological interventions. There isn’t a one-size-fits-all solution, but here are some strategies to consider:
-
Stress Management Techniques: Incorporate stress-reducing practices into your daily routine. These could include:
- Mindfulness meditation: Even 5-10 minutes per day can make a difference.
- Deep breathing exercises: Simple diaphragmatic breathing helps calm the nervous system.
- Yoga or Tai Chi: Combines physical movement with mindful awareness.
- Progressive muscle relaxation: Systematically tensing and relaxing different muscle groups.
-
Physical Therapies:
- TMJ therapy: A skilled therapist can help release tension in the jaw muscles, improve range of motion, and correct postural imbalances.
- Massage Therapy: Targeting neck, shoulder, and back muscles can alleviate tension radiating from the jaw.
-
Postural Correction Exercises: Strengthening core muscles and improving posture reduces abdominal pressure and supports esophageal function.
-
Behavioral Modifications:
- Awareness of Clenching: Pay attention to when you clench your jaw – during stressful situations, while working on a computer, or even in your sleep. This self-awareness is the first step towards change.
- Conscious Relaxation: Practice consciously relaxing your jaw throughout the day. Gently separate your teeth and allow your jaw to rest.
- Dietary Adjustments: Identify and eliminate GERD trigger foods (spicy foods, caffeine, alcohol, chocolate, etc.).
- Sleep Hygiene: Optimize sleep patterns as poor sleep exacerbates stress and clenching. GERD and Sleep Apnea can disrupt rest.
Ultimately, breaking the stress-reflux loop is about regaining control over your body and mind. It’s a journey that requires patience, self-compassion, and a willingness to explore different approaches until you find what works best for you. Remember, seeking guidance from healthcare professionals – doctors, therapists, physical therapists – is crucial for developing a personalized plan tailored to your specific needs and circumstances.
Beyond the Basics: Exploring Advanced Interventions
While lifestyle adjustments are often the first line of defense, some individuals may benefit from more advanced interventions. These should always be discussed with a qualified healthcare provider, as they vary in suitability depending on the severity of symptoms and underlying factors. Biofeedback is one such option. It involves using sensors to monitor physiological responses like muscle tension (in the jaw or neck) and heart rate variability. This real-time feedback allows individuals to learn how to consciously control these responses, reducing tension and promoting relaxation.
Another potential avenue is cognitive behavioral therapy for bruxism (CBT-B). This type of therapy focuses on identifying and modifying thoughts and behaviors that contribute to jaw clenching. It often includes techniques like stress management training, sleep hygiene education, and habit reversal training (learning alternative behaviors to replace clenching). CBT-B can be particularly effective for individuals whose bruxism is linked to anxiety or trauma.
Finally, in some cases, a mouth guard might be recommended by a dentist. While mouth guards don’t address the underlying cause of jaw clenching, they can protect teeth from damage and reduce muscle fatigue. However, it’s important to note that relying solely on a mouth guard without addressing stress and other contributing factors may not provide long-term relief. The most effective approach is typically a combination of interventions tailored to the individual’s specific needs.
It’s also crucial to rule out other potential causes for both GERD and bruxism. Sometimes, seemingly unrelated medical conditions or medications can contribute to these symptoms. A thorough evaluation by healthcare professionals is essential for accurate diagnosis and appropriate treatment planning. Acid reflux and nausea should be investigated as well. If you experience hiccups, consider The connection between GERD and Hiccups. Also, be aware of the connection between GERD and throat clearing.