Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide. Most people associate it with heartburn, that burning sensation in the chest after a meal, but its effects can be far more widespread and subtle than many realize. Beyond the typical discomfort, GERD can manifest in a variety of unusual ways, including feelings of muscle weakness or fatigue after eating. This isn’t simply about digestive upset; it speaks to the complex interplay between our gut, nervous system, and overall physical wellbeing. Understanding why this happens requires delving into the mechanisms behind both GERD and its potential impact on neuromuscular function.
The connection between GERD and muscle weakness often goes unrecognized because it’s not a direct, immediate symptom like acid reflux itself. It’s more insidious, building over time as chronic inflammation or nutrient malabsorption takes hold. This can lead to individuals questioning their fitness levels or attributing the weakness to other causes, leading to delayed diagnosis and potentially ineffective management strategies. The experience is also highly variable; some may feel a general sense of fatigue, while others report specific muscle groups feeling weaker after meals, particularly those rich in fats or carbohydrates. Recognizing this potential link is crucial for holistic health assessment and treatment planning. If you are feeling tired after eating it’s important to seek help.
Understanding the GERD-Muscle Weakness Link
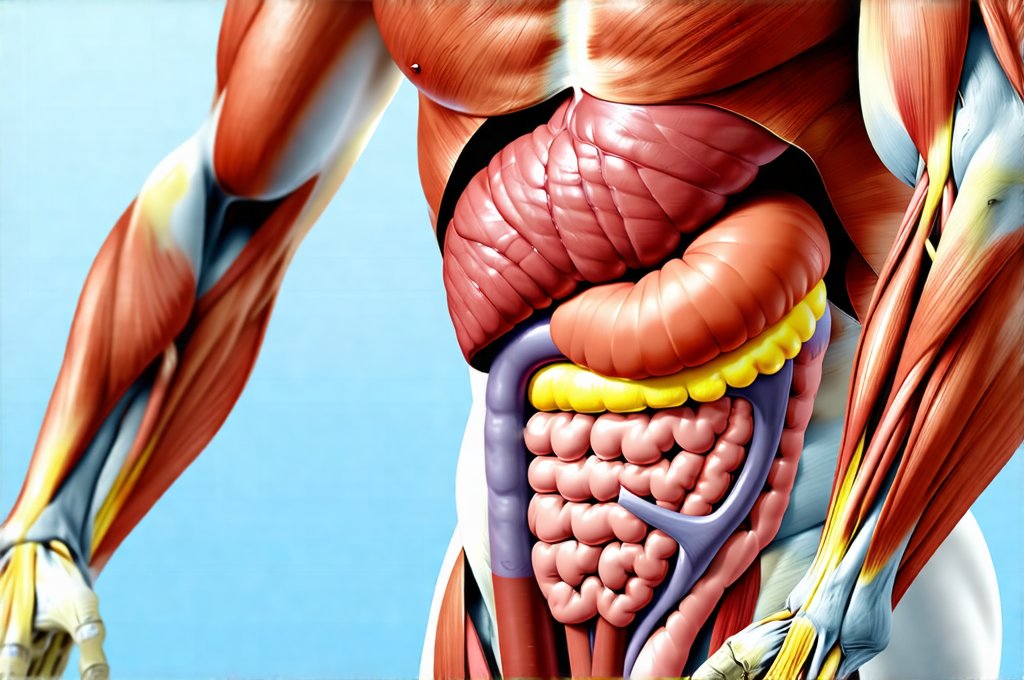
The relationship between GERD and muscle weakness isn’t straightforward; it’s a multifaceted issue with several contributing factors. At its core, chronic GERD induces persistent low-grade inflammation throughout the body. This inflammation doesn’t stay localized to the esophagus – it can seep into systemic circulation, affecting various organs and tissues, including muscles. Inflammatory cytokines released as part of the reflux process disrupt normal muscle function and energy production. Furthermore, frequent acid exposure can damage the esophageal lining, leading to nutrient malabsorption, particularly of vital vitamins and minerals crucial for muscle health like Vitamin D, Magnesium, and Iron. This deficiency exacerbates weakness.
The vagus nerve plays a significant role in this connection too. GERD often causes irritation and inflammation that impacts vagal tone – the activity level of the vagus nerve, which is central to the parasympathetic nervous system responsible for ‘rest and digest’ functions. A compromised vagus nerve can lead to diminished muscle control, fatigue, and reduced energy levels. It also affects digestive processes further worsening nutrient absorption. This creates a vicious cycle where GERD causes inflammation, impacts the vagus nerve, hinders digestion, leads to nutrient deficiencies, and ultimately contributes to muscle weakness.
Finally, consider the behavioral aspect. Individuals with chronic GERD might alter their eating habits – avoiding certain foods or reducing intake altogether – leading to inadequate caloric and nutritional support for optimal muscle function. The constant discomfort can also lead to decreased physical activity, further accelerating muscle loss and weakness. This highlights how GERD’s impact extends beyond the purely physiological realm. It’s important to cope with fatigue that comes along with this condition.
Nutritional Deficiencies & Muscle Function
Muscle strength and endurance are heavily reliant on adequate nutrient intake. Several key nutrients are often compromised in individuals with long-standing GERD due to malabsorption or dietary restrictions aimed at managing symptoms.
- Vitamin D: Essential for muscle protein synthesis and neuromuscular function. Low levels directly correlate with muscle weakness and increased risk of falls, especially in older adults.
- Magnesium: Plays a vital role in muscle contraction and relaxation. Deficiency can cause muscle cramps, spasms, and overall weakness. GERD medications like proton pump inhibitors (PPIs) can further deplete magnesium levels.
- Iron: Critical for oxygen transport to muscles. Iron deficiency anemia leads to fatigue, reduced exercise capacity, and generalized weakness. Chronic inflammation from GERD can also impair iron absorption.
- Vitamin B12: Necessary for nerve function and red blood cell production. Malabsorption due to impaired digestion or long-term PPI use can result in B12 deficiency, contributing to neurological symptoms including muscle fatigue and weakness.
Addressing these deficiencies through diet (where possible) or appropriate supplementation – under the guidance of a healthcare professional – is crucial for restoring muscle function. It’s important to note that self-supplementation isn’t always advisable; excessive intake can sometimes be harmful, and accurate diagnosis of deficiencies is essential before starting any regimen. If you experience bloating after eating, this could also indicate a nutritional deficiency.
The Role of Inflammation & Cytokines
Chronic inflammation is the common denominator linking GERD to a wide range of systemic health problems, including muscle weakness. When stomach acid frequently backflows into the esophagus, it triggers an inflammatory response. This isn’t just limited to the esophageal lining; the body releases cytokines – signaling molecules that mediate inflammation – into circulation.
These cytokines have far-reaching effects:
* Muscle Protein Breakdown: Some cytokines promote muscle protein breakdown, leading to loss of muscle mass and strength.
* Mitochondrial Dysfunction: Inflammation can disrupt mitochondrial function within muscle cells, reducing their ability to produce energy (ATP). This results in fatigue and weakness.
* Neuromuscular Junction Interference: Chronic inflammation can interfere with the neuromuscular junction – the site where nerves communicate with muscles – impairing nerve transmission and causing weakness.
Managing GERD effectively to reduce inflammation is therefore a key strategy for mitigating muscle weakness. Lifestyle modifications, dietary changes, and appropriate medication (as prescribed by a doctor) are all vital components of this approach. It’s also important to recognize that other sources of chronic inflammation – such as poor diet or stress – can exacerbate the problem, creating a cumulative effect. Digestive discomfort can be an indicator of underlying inflammation.
Vagal Tone & Neuromuscular Control
As previously mentioned, the vagus nerve is intimately involved in regulating digestive function and has significant influence over neuromuscular control. GERD-induced esophageal irritation can impact vagal tone, leading to diminished parasympathetic activity. This disruption contributes to several factors that cause muscle weakness:
- Reduced Muscle Blood Flow: The vagus nerve helps regulate blood flow to muscles. Lowered vagal tone can constrict blood vessels, reducing oxygen and nutrient delivery to muscles.
- Impaired Nerve Function: Vagal dysfunction directly affects the nervous system’s ability to properly signal muscle contraction and relaxation.
- Increased Stress Response: A compromised vagus nerve often leads to increased sympathetic nervous system activity (the ‘fight or flight’ response), which can contribute to muscle tension, fatigue, and overall weakness.
Techniques aimed at increasing vagal tone – such as deep breathing exercises, meditation, yoga, cold water immersion, and even singing – may offer a complementary approach to managing GERD-related muscle weakness. However, these techniques should not replace conventional medical treatment and are best used in conjunction with it. A healthcare professional can help determine the appropriate strategies based on individual needs and health status. In some instances, employment may need to be adjusted to accommodate these symptoms.
It is vital to remember that this information provides general knowledge and should not be interpreted as medical advice. If you suspect a link between GERD and muscle weakness, consult your doctor for proper diagnosis and treatment. Self-treating can delay appropriate care and potentially worsen your condition. If digestive issues occur after surgery it is important to seek medical advice.