Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide, often characterized by frequent heartburn and acid regurgitation. However, the experience of GERD can be incredibly diverse, extending beyond these typical symptoms to include more unusual sensations. One such sensation that many individuals report is a peculiar “bubble” or globus-like feeling in the esophagus – a discomfort that can range from mildly annoying to profoundly unsettling. This isn’t necessarily about pain; it’s often described as a tightness, fullness, or the distinct sense of something being lodged in the throat or chest, making swallowing difficult or causing chronic clearing of the throat. Understanding this less-recognized manifestation of GERD is crucial for accurate diagnosis and effective management.
The sensation can be particularly frustrating because it often doesn’t respond to typical over-the-counter remedies for heartburn. This leads many people to question whether their symptoms are even related to GERD at all, or if something more serious is occurring. It’s important to remember that the human digestive system is a complex network and variations in how individuals experience its malfunctions are entirely normal. The ‘bubble’ sensation isn’t always indicative of severe disease, but it should be investigated by a healthcare professional to rule out other potential causes and determine the best course of action. This article will delve into the connection between GERD and this specific symptom, exploring possible mechanisms, associated factors, and strategies for finding relief.
The Link Between GERD and Esophageal Sensations
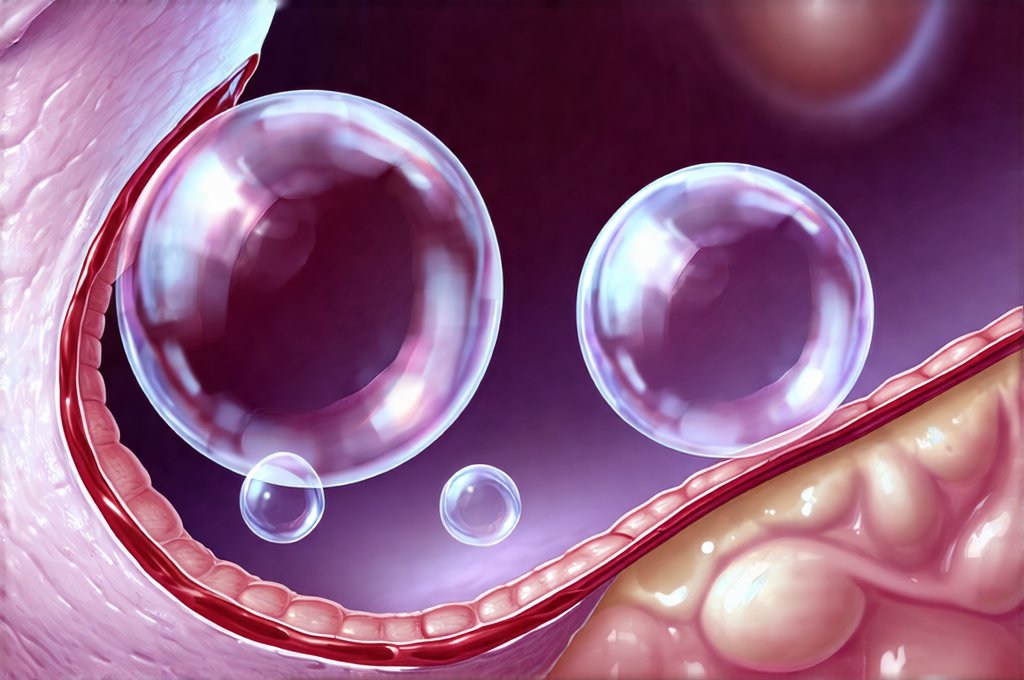
The sensation of a ‘bubble’ in the esophagus is often closely tied to the underlying physiological processes of GERD, even if acid reflux isn’t always present or perceived as typical heartburn. While classic GERD symptoms involve stomach acid irritating the esophageal lining, visceral hypersensitivity plays a significant role for many individuals. This means that the esophagus becomes abnormally sensitive to even normal amounts of acid or pressure, leading to heightened discomfort and unusual sensations. The bubble feeling can be a direct result of this increased sensitivity; minor fluctuations in esophageal motility or even gas can be interpreted as something more substantial.
The lower esophageal sphincter (LES) is a muscular ring at the bottom of the esophagus that prevents stomach contents from flowing back up. In GERD, the LES weakens or relaxes inappropriately, allowing acid and other substances to reflux into the esophagus. This constant irritation and inflammation can alter nerve function in the esophagus, contributing to hypersensitivity. Even when there’s no actual reflux happening, the brain may perceive a sensation due to these altered neural pathways. The bubble feeling could be your nervous system misinterpreting normal esophageal contractions or peristalsis (the wave-like muscle movements that move food down) as something obstructing the passage.
Furthermore, GERD can lead to inflammation and changes in the esophageal lining itself. This can affect how the esophagus functions mechanically, leading to difficulties with swallowing – a condition known as dysphagia – and contributing to the sensation of fullness or obstruction. The feeling isn’t necessarily about a physical bubble; it’s often the brain interpreting signals from an irritated or dysfunctional esophagus as something being present where it shouldn’t be. This explains why many people describe the sensation as similar to having a lump in their throat, even though there is nothing physically obstructing the airway. Understanding the role of bile can also provide insight into digestive discomfort.
Understanding Globus Sensation and its Relation to GERD
Globus sensation, often described as a persistent feeling of a lump or foreign body in the throat, can frequently mimic the ‘bubble’ sensation experienced by those with GERD. While globus isn’t always directly linked to gastrointestinal issues, there is significant overlap and co-occurrence with GERD. It’s important to differentiate between these two conditions because their underlying causes and approaches to management differ somewhat. Globus sensation often stems from muscle tension in the throat or upper esophageal sphincter (UES) and is frequently associated with stress or anxiety.
However, GERD can contribute to globus sensation through several mechanisms. Chronic acid reflux can irritate the esophagus and UES, leading to muscle spasms and dysfunction. This creates a feeling of tightness or obstruction, similar to having something stuck in the throat. Moreover, the constant discomfort from GERD may lead to increased stress and anxiety, which are known triggers for globus sensation. Therefore, it’s not always easy to determine whether the globus is solely psychological or has a physiological basis linked to GERD. Meal timing can also impact these symptoms.
Diagnosing the difference often requires careful evaluation by a healthcare professional. This might involve: 1) A thorough medical history focusing on reflux symptoms, stress levels, and swallowing difficulties; 2) Physical examination of the throat and esophagus; 3) Possible diagnostic tests like endoscopy (to visualize the esophagus), manometry (to measure esophageal pressure), and pH monitoring (to detect acid reflux). It’s crucial to rule out other causes of globus sensation, such as thyroid problems or esophageal tumors, before attributing it solely to GERD. Consider also understanding antacids for symptomatic relief.
The Role of Esophageal Motility Disorders
Esophageal motility disorders are conditions that affect the ability of the esophagus to effectively move food and liquids from the throat to the stomach. These disorders can significantly contribute to the ‘bubble’ feeling in several ways. Achalasia, for example, is a rare disorder where the LES fails to relax properly, making it difficult for food to pass through. While achalasia usually presents with more pronounced dysphagia (difficulty swallowing), even mild forms of motility dysfunction can create a sensation of fullness or obstruction that mimics a bubble in the esophagus.
Another common motility issue is nutcracker esophagus, where the esophageal muscles contract too forcefully during swallowing, causing chest pain and discomfort. These strong contractions can be perceived as tightness or pressure in the chest and throat, leading to the ‘bubble’ sensation. Even more subtle disruptions in esophageal peristalsis – the rhythmic wave-like muscle movements that propel food down – can create a sense of incomplete emptying or lingering fullness.
Importantly, GERD can exacerbate existing motility disorders and even contribute to their development. Chronic acid exposure can damage the nerves controlling esophageal muscles, leading to dysfunction over time. This creates a vicious cycle: GERD causes inflammation, which disrupts motility, which worsens GERD symptoms. Diagnosing these motility disorders requires specialized testing like esophageal manometry, and treatment often involves lifestyle modifications, medications to reduce reflux, or in some cases, surgical intervention. Weight management can play a significant role here as well.
Lifestyle Modifications and Management Strategies
While the sensation of a ‘bubble’ in the esophagus can be unsettling, there are several strategies that can help manage it effectively. Lifestyle modifications are often the first line of defense, particularly for those with mild to moderate GERD. These include: – Elevating the head of your bed by 6-8 inches; – Avoiding trigger foods like caffeine, alcohol, chocolate, and fatty meals; – Eating smaller, more frequent meals; – Losing weight if overweight or obese; – Quitting smoking.
Dietary changes can also play a role. Identifying and eliminating foods that worsen your symptoms is key. Keeping a food diary can help pinpoint these triggers. Consider incorporating fiber-rich foods to promote healthy digestion and avoiding overly processed foods. Stress management techniques, such as yoga, meditation, or deep breathing exercises, are crucial because stress can exacerbate GERD symptoms and contribute to globus sensation. Chewing gum is another potential aid in symptom management.
Medications might be necessary for more severe cases. Over-the-counter antacids can provide temporary relief from heartburn, but proton pump inhibitors (PPIs) or H2 receptor antagonists may be prescribed by your doctor to reduce acid production if lifestyle changes aren’t enough. If motility disorders are diagnosed, specific medications to improve esophageal muscle function might also be recommended. It’s vital to consult a healthcare professional before starting any new medication regimen. Finally, remember that seeking support from friends, family, or a therapist can significantly help cope with the emotional distress associated with chronic GERD symptoms and unusual sensations like the ‘bubble’ feeling. FODMAPs should also be considered in relation to digestive discomfort.