Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide. Many people experience occasional heartburn or acid indigestion after a large meal – this is normal. However, when these symptoms become frequent and intense, interfering with daily life, it could signal GERD. Beyond the hallmark burning sensation in the chest, many individuals also report experiencing noticeable stomach noises—gurgling, rumbling, or even loud splashing sounds. These sounds can be unsettling and raise a fundamental question: are they simply a normal part of digestion, or do they indicate something more serious related to GERD? Understanding the connection between these two phenomena is crucial for appropriate self-care and knowing when to seek medical attention.
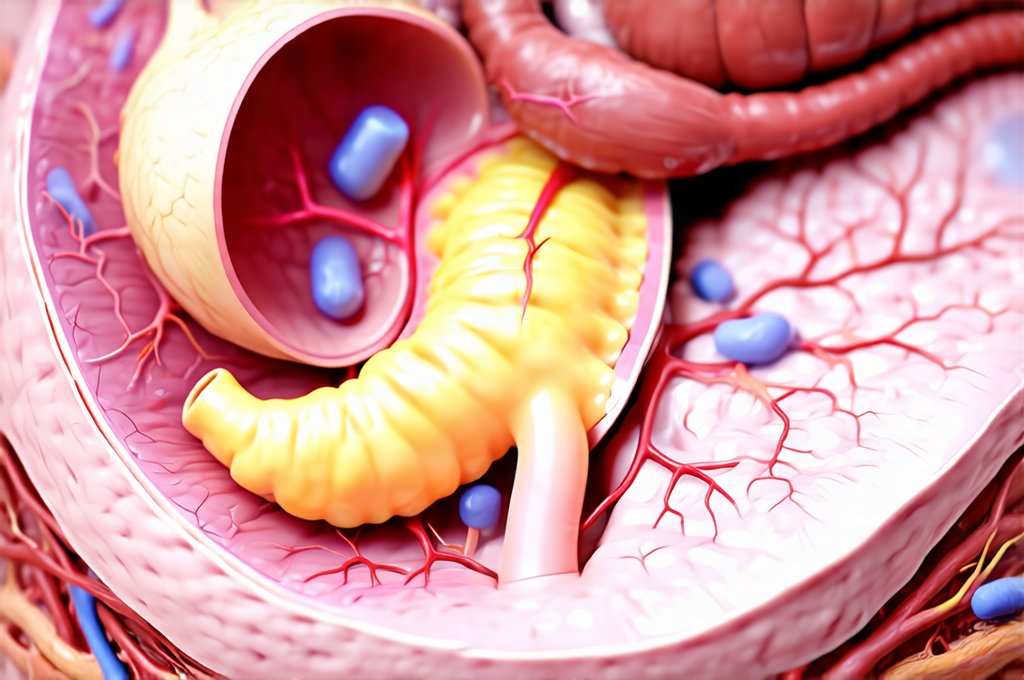
The digestive system is inherently noisy; it’s constantly working to break down food, mixing fluids, and moving contents along the gastrointestinal tract. These processes naturally produce sounds, often referred to as borborygmi. However, a significant increase in these noises, or changes in their character coupled with GERD symptoms, can be indicative of underlying issues. It’s important to differentiate between normal digestive sounds and those that warrant further investigation. This article will explore the relationship between GERD and loud stomach noises, helping you understand when they are likely harmless and when a consultation with a healthcare professional is advisable. We’ll delve into the mechanisms behind both conditions and discuss potential management strategies.
The Link Between GERD and Digestive Sounds
GERD arises from a weakening or malfunction of the lower esophageal sphincter (LES), the muscular valve that prevents stomach acid from flowing back up into the esophagus. When this happens, acid reflux occurs, leading to heartburn, regurgitation, and other uncomfortable symptoms. But how does this relate to increased digestive noises? The answer lies in the disruption of normal digestive processes caused by GERD and its associated inflammation. Chronic acid exposure irritates the esophageal lining, potentially affecting motility – the coordinated muscle contractions that move food through the digestive tract. This can lead to delayed gastric emptying, meaning food stays in the stomach longer.
A fuller stomach for an extended period naturally increases gas production and intestinal activity as the body attempts to process the food. This increased activity generates more sounds. Moreover, GERD often leads to bloating and distension, which further amplify these noises. Some individuals also develop aerophagia, swallowing excessive air, either consciously or unconsciously, in response to discomfort or anxiety associated with GERD symptoms – contributing to even greater gas production and audible digestive activity. It’s a complex interplay where the reflux itself exacerbates normal digestive sounds, making them more noticeable and potentially concerning.
Finally, it’s important to note that medications used to manage GERD can sometimes contribute to changes in digestive sounds. For example, proton pump inhibitors (PPIs), while effective at reducing acid production, may alter gut microbiota and affect digestion differently, potentially leading to increased gas or altered motility patterns over time. These effects are not universal, but they represent another layer of complexity in understanding the connection between GERD and stomach noises. If you’re being taken seriously with normal bloodwork and pain, it’s important to explore all options.
Identifying Concerning Noises vs. Normal Digestion
Distinguishing between normal digestive sounds and those that may indicate a problem requires careful observation and self-awareness. As mentioned earlier, borborygmi—the rumbling and gurgling sounds produced during digestion—are perfectly normal. They usually occur after eating and are not accompanied by pain or other concerning symptoms. However, certain characteristics should raise red flags. Loud, persistent noises that sound like splashing, roaring, or contain a distinct high-pitched tone could be indicative of an underlying issue beyond simple GERD.
Pay attention to when the sounds occur. Are they consistently present even when you haven’t eaten? Do they happen specifically after meals, and if so, are they significantly louder or different in character than usual? Are they accompanied by other symptoms like abdominal pain, bloating, nausea, vomiting, diarrhea, constipation, unintended weight loss, or difficulty swallowing (dysphagia)? The presence of these accompanying symptoms suggests the issue may be more serious than GERD alone. Furthermore, a sudden change in your typical digestive sounds should always prompt attention – if your stomach has been relatively quiet and then suddenly becomes very noisy, it’s worth exploring the cause with a healthcare professional.
It’s also important to consider that anxiety can amplify perceived noises. Stress and worry about GERD symptoms themselves can lead to increased awareness of normal bodily functions, making digestive sounds seem more prominent than they actually are. Learning relaxation techniques and managing stress levels can sometimes help reduce this heightened perception. However, if the noises persist despite stress management efforts, medical evaluation is still necessary.
Understanding Potential Underlying Causes Beyond GERD
While GERD can certainly contribute to loud stomach noises, it’s crucial to remember that other conditions can cause similar symptoms. Irritable bowel syndrome (IBS) is a common gastrointestinal disorder characterized by abdominal pain, bloating, gas, diarrhea, and constipation – all of which can generate significant digestive sounds. Food intolerances or allergies, such as lactose intolerance or celiac disease, can also lead to increased gas production and noisy digestion. Small intestinal bacterial overgrowth (SIBO) is another possibility where an excessive amount of bacteria in the small intestine ferments undigested food, creating gas and bloating.
These conditions often overlap with GERD symptoms, making diagnosis challenging. For example, IBS frequently co-occurs with GERD, and both can be exacerbated by stress and dietary factors. A healthcare professional will need to consider all possible causes when evaluating your symptoms. This may involve a thorough medical history, physical examination, and potentially diagnostic tests such as:
- Endoscopy: To visualize the esophagus and stomach for signs of inflammation or damage.
- Breath tests: To detect SIBO or lactose intolerance.
- Stool analysis: To identify potential infections or malabsorption issues.
- Food allergy/intolerance testing: Although these are often controversial, they can sometimes be helpful in identifying trigger foods.
If you have signs your stomach trouble isn’t an ulcer or cancer, it’s important to seek medical attention.
Dietary and Lifestyle Modifications for Relief
Regardless of the underlying cause, certain dietary and lifestyle modifications can often help alleviate both GERD symptoms and associated digestive noises. – Dietary changes are paramount. Identifying and eliminating trigger foods – such as fatty foods, spicy foods, caffeine, alcohol, chocolate, and acidic foods (tomatoes, citrus fruits) – can significantly reduce acid reflux and subsequent bloating. Eating smaller, more frequent meals instead of large ones minimizes the amount of stomach contents and reduces pressure on the LES.
– Lifestyle adjustments are also essential. Elevating the head of your bed by 6-8 inches can help prevent nighttime reflux. Avoiding eating within 2-3 hours of bedtime allows the stomach to empty before lying down. Maintaining a healthy weight, quitting smoking, and managing stress levels all contribute to improved digestive health. If you’re dealing with K21.9 — GERD without esophagitis, these modifications can be particularly helpful.
When to Seek Medical Attention
While many cases of loud stomach noises associated with GERD can be managed with self-care measures, it’s important to know when to seek professional help. Do not delay seeking medical attention if you experience any of the following: – Severe abdominal pain that is constant or worsening.
– Persistent nausea and vomiting.
– Difficulty swallowing (dysphagia).
– Unintentional weight loss.
– Blood in your stool or vomit.
– New or worsening GERD symptoms despite lifestyle modifications and over-the-counter medications.
– Significant changes in bowel habits (diarrhea, constipation) that persist for more than a few days.
A healthcare professional can accurately diagnose the underlying cause of your symptoms and recommend appropriate treatment options, which may include prescription medications to reduce acid production, manage motility issues, or address any coexisting gastrointestinal conditions. Remember, self-diagnosis can be risky; consulting with a medical expert is the best way to ensure you receive proper care and avoid complications. You should also consider if K31.9 — stomach condition could be causing your symptoms. Finally, understanding K21.0 — GERD with esophagitis can help you better understand your condition.