Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide, often manifesting as persistent heartburn, regurgitation, or even seemingly unrelated symptoms like chronic cough or hoarseness. While many associate GERD with dietary factors and stress, the intricate relationship between this digestive issue and proper hydration frequently gets overlooked. Maintaining adequate fluid intake isn’t just about quenching thirst; it plays a vital role in overall health, and crucially, impacts the functioning of the esophageal sphincter, stomach acid production, and even the composition of gastric contents – all key players in the GERD equation. Understanding how these elements interact can empower individuals to proactively manage their symptoms and improve their quality of life.
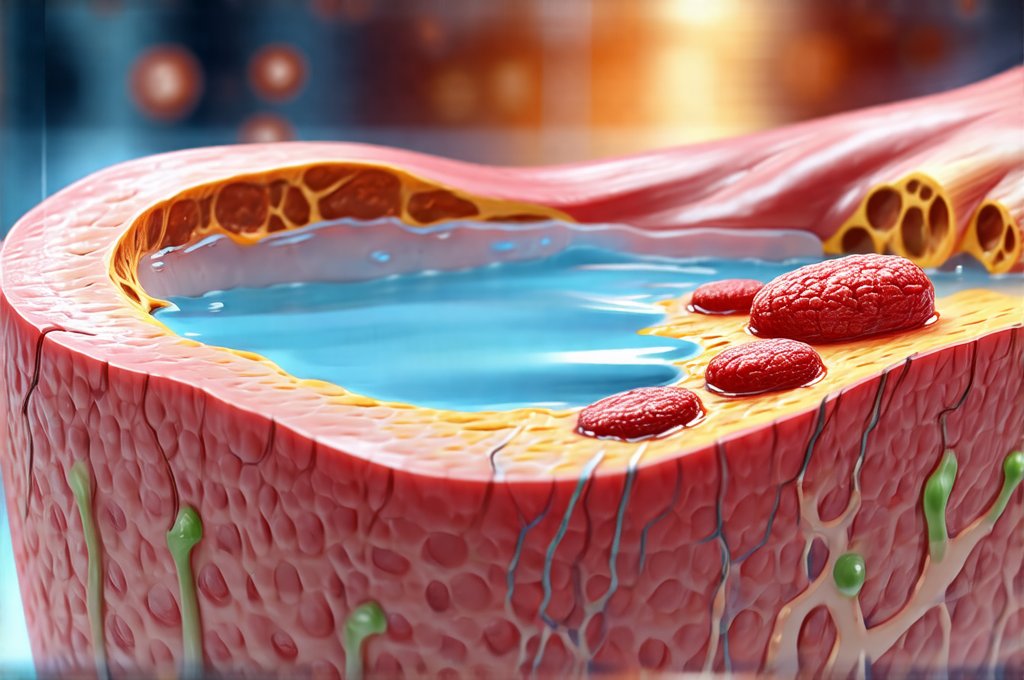
The digestive process relies heavily on water for efficient function. When we’re dehydrated, our bodies attempt to conserve fluids, sometimes leading to a thicker, more concentrated stomach acid environment. This heightened acidity can exacerbate reflux episodes and increase esophageal irritation. Furthermore, dehydration affects the motility—the movement of food through the digestive tract—potentially slowing it down and increasing the risk of backflow. It’s a complex interplay where seemingly minor fluctuations in hydration levels can significantly influence GERD symptoms. This article will delve into the specific ways GERD and dehydration are linked, offering insights into practical strategies for staying hydrated while managing this condition effectively.
The Bidirectional Relationship: How GERD Impacts Hydration & Vice Versa
GERD isn’t simply caused by dehydration, nor does dehydration always lead to GERD; it’s far more nuanced than that. There exists a bidirectional relationship where each can influence the other, creating a potentially vicious cycle. Chronic acid reflux can actually contribute to dehydration in several ways. Frequent regurgitation, especially if voluminous, results in fluid loss. While seemingly minimal per episode, these losses accumulate over time. Additionally, some individuals with GERD experience nausea or difficulty swallowing (dysphagia), leading them to reduce their fluid intake voluntarily as a way to avoid discomfort. This reduction then exacerbates the reflux symptoms, furthering dehydration.
On the other hand, as previously mentioned, dehydration itself can worsen acid reflux. A dehydrated body produces more concentrated stomach acid which is harsher on the esophageal lining during reflux episodes. Reduced saliva production due to dehydration also contributes, because saliva naturally neutralizes stomach acid and helps clear the esophagus. Finally, the slower digestive motility associated with dehydration increases the likelihood of prolonged food retention in the stomach, creating a greater chance for backflow. This creates a feedback loop: GERD leads to potential fluid loss or reduced intake, which worsens GERD symptoms, and so on.
Recognizing this interplay is vital for effective management. It’s not enough to simply address the reflux; attention must also be paid to maintaining optimal hydration levels. This requires a conscious effort to drink sufficient fluids throughout the day, even when symptoms are present, and choosing beverages that support digestive health rather than exacerbate it.
Optimizing Hydration with GERD: What To Drink & Avoid
The type of fluid consumed is as important as the quantity. While water remains the gold standard for hydration, certain other beverages can either help or hinder symptom management. Plain water should be your primary source of fluids – aim for at least 8 glasses a day, adjusting based on activity level and climate. Herbal teas (like chamomile or ginger) can also be soothing and hydrating, but avoid those with caffeine or mint, as these can potentially relax the lower esophageal sphincter. Coconut water is another excellent option providing electrolytes which are often lost during reflux episodes.
Conversely, several beverages are known to worsen GERD symptoms and should be limited or avoided:
* Caffeinated drinks: Coffee, tea, and energy drinks can increase acid production and weaken the LES.
* Alcohol: Alcohol relaxes the LES, allowing stomach acid to flow back into the esophagus.
* Carbonated beverages: The bubbles in carbonated drinks can increase pressure in the stomach, leading to reflux.
* Citrus juices: Highly acidic citrus fruits may irritate the esophageal lining.
* Full-fat milk: While seemingly benign, full-fat dairy products can sometimes exacerbate symptoms in some individuals due to their slow digestion and potential for increased acid production.
It’s important to note that individual tolerance varies significantly. What triggers one person’s GERD might not affect another. Keeping a food diary to track fluid intake alongside symptom occurrence can help identify personal trigger beverages.
The Role of Electrolytes in GERD & Hydration
Electrolytes—sodium, potassium, magnesium, and chloride—are crucial for maintaining proper fluid balance within the body. When you experience reflux or regurgitation, some electrolytes are lost along with fluids. This imbalance can contribute to dehydration symptoms like fatigue, muscle cramps, and even dizziness, which can be mistaken for other GERD-related issues. Restoring electrolyte balance is therefore a key component of managing hydration alongside GERD.
Simple strategies for replenishing electrolytes include:
1. Consuming electrolyte-rich beverages such as coconut water or sports drinks (in moderation due to sugar content).
2. Incorporating foods naturally high in electrolytes into your diet, like bananas (potassium), spinach (magnesium), and pickles/olives (sodium – consume cautiously if you have blood pressure concerns).
3. Considering oral rehydration solutions specifically formulated for mild dehydration – these often provide a balanced electrolyte profile without excessive sugar.
However, it’s essential to avoid overdoing electrolyte intake, particularly sodium, as excess sodium can contribute to fluid retention and potentially worsen GERD symptoms in some individuals. A balanced approach is crucial.
Hydration & Medication Interactions
Many people with GERD rely on medications like proton pump inhibitors (PPIs) or H2 receptor antagonists to manage their symptoms. While these medications effectively reduce acid production, they don’t address the underlying hydration issues that can contribute to reflux. In fact, some PPIs have been linked to potential electrolyte imbalances, specifically magnesium levels. Long-term use of PPIs can sometimes impair magnesium absorption, leading to deficiency and potentially exacerbating GERD symptoms or causing other health problems.
It’s vital to discuss your medication regimen with your doctor and inquire about potential interactions with hydration status. If you’re on a long-term PPI, consider getting your magnesium levels checked periodically. Staying adequately hydrated can help mitigate some of these effects by supporting overall kidney function and electrolyte absorption. Additionally, understanding that medications address the symptoms of GERD, not the root cause, emphasizes the importance of lifestyle modifications like proper hydration as a cornerstone of long-term management. If you experience gastritis alongside GERD, this is even more important.
Practical Tips for Increasing Fluid Intake
Many people struggle to drink enough water throughout the day, even without GERD complicating matters. Here are some practical tips to increase your fluid intake:
* Carry a reusable water bottle with you at all times and sip on it regularly.
* Set reminders on your phone or computer to prompt you to drink water.
* Drink a glass of water before each meal – this can also help dilute stomach acid.
* Infuse your water with fruits like lemon, cucumber, or berries for added flavor (avoid citrus if it triggers symptoms).
* Choose hydrating snacks like watermelon, cucumbers, or celery sticks.
* Track your fluid intake to ensure you’re meeting your daily goals.
Remember: Listen to your body and adjust your hydration strategies based on your individual needs and tolerance levels. Staying adequately hydrated is a proactive step towards managing GERD symptoms and improving overall well-being. If dietary sensitivities are also a concern, explore what happens when you eat foods that trigger your reflux. Consider whether avoiding fruit might also help manage symptoms. And be mindful of lectins in beans, which can contribute to digestive distress.
Disclaimer: This article provides general information about GERD and dehydration and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis, treatment, and personalized recommendations regarding your health condition.