The chest – a seemingly simple area of the body, yet one capable of hosting an extraordinary range of sensations, both physical and emotional. Often, when discomfort arises in this region, it triggers immediate concern, fueled by understandable anxieties about heart health or more serious conditions. However, many experiences categorized as alarming are, in fact, manifestations of either gastroesophageal reflux disease (GERD) or panic attacks – two distinct phenomena that can mimic each other with unsettling accuracy. This similarity often leads to confusion and unnecessary worry, prompting individuals to seek emergency medical attention or self-diagnose incorrectly. Understanding the nuances between these conditions is crucial for appropriate response and management, ensuring both physical and mental well-being.
The challenge in differentiating GERD from a panic attack lies in their overlapping symptoms. Chest pain, difficulty breathing, a racing heart – all commonly experienced in both scenarios. This overlap isn’t surprising; the vagus nerve connects the gut and the brain, creating a powerful bidirectional communication pathway. What happens physically in one area can profoundly impact the other, leading to complex symptom presentations. Moreover, anxiety itself can exacerbate GERD symptoms, and conversely, chronic discomfort from GERD can heighten anxiety levels, creating a feedback loop that makes pinpointing the root cause incredibly difficult. This article aims to dissect these conditions, exploring their individual characteristics, common triggers, and potential methods for self-assessment (though it emphatically stresses the importance of consulting with healthcare professionals for any concerning symptoms). If you are prone to reactivity while eating, consider how to eat peacefully to minimize discomfort.
Understanding GERD & Panic Attacks: Core Differences
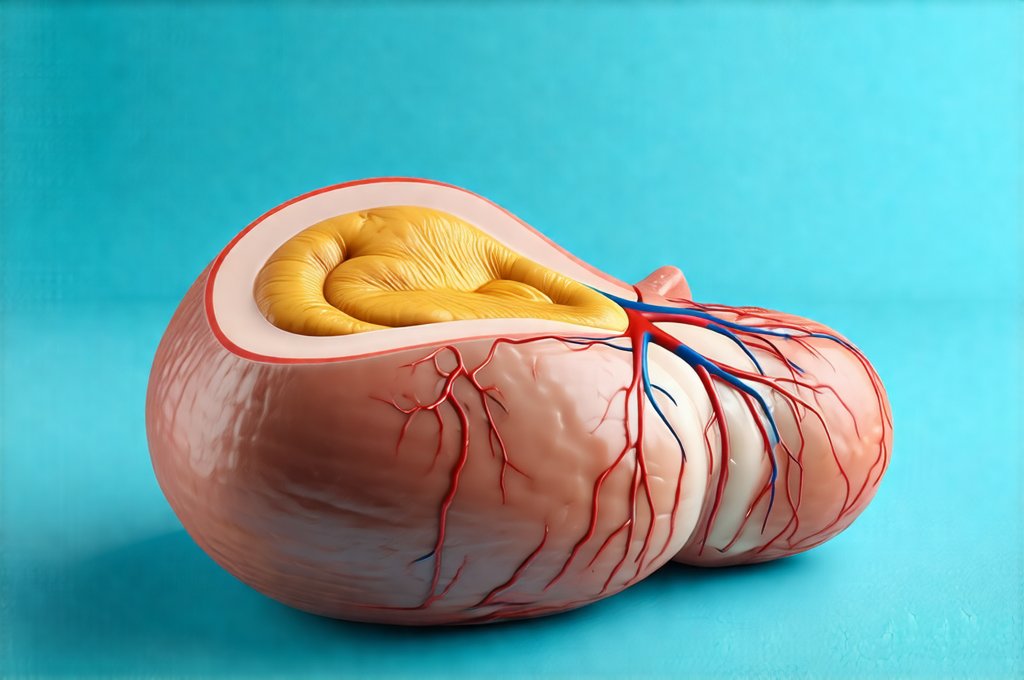
Gastroesophageal reflux disease (GERD) is a chronic digestive disorder characterized by the frequent backflow of stomach acid into the esophagus. This acidic reflux irritates the esophageal lining, leading to a variety of symptoms beyond just heartburn. These can include chest pain that often mimics cardiac issues, difficulty swallowing (dysphagia), a persistent cough, hoarseness, and even asthma-like symptoms. The underlying cause is typically a weakened lower esophageal sphincter (LES) – the muscular valve that prevents stomach contents from traveling upward. Lifestyle factors like diet, obesity, smoking, and certain medications can contribute to GERD development. It’s fundamentally a physical condition rooted in digestive processes. Sometimes a gentle gut cleanse can help reset the system.
In contrast, a panic attack is an intense surge of fear or discomfort accompanied by physical symptoms such as heart palpitations, shortness of breath, dizziness, trembling, sweating, and – crucially – chest pain. Panic attacks are a core feature of panic disorder, but can also occur in other anxiety disorders or even in individuals without a diagnosed mental health condition. Unlike GERD, which stems from a physiological issue, panic attacks originate within the nervous system and represent an overactivation of the body’s fight-or-flight response. They are often triggered by perceived threats (real or imagined) but can also arise seemingly out of nowhere.
The key distinction lies in the origin and nature of the symptoms. GERD pain is generally described as a burning sensation behind the breastbone, often worsening after eating or lying down. Panic attack chest pain tends to be sharper, more stabbing, and less related to food intake. It’s also frequently accompanied by an overwhelming sense of dread or impending doom – a hallmark characteristic of panic attacks that rarely accompanies GERD. However, these are generalizations, and the overlap is substantial enough to make self-diagnosis unreliable. If you struggle with digestive discomfort after eating certain foods, it might be helpful to learn how to enjoy spices without triggering symptoms.
Recognizing Triggers & Symptom Patterns
Identifying what sets off each condition can provide valuable clues for differentiation. For GERD, common triggers include: – Spicy foods – Fatty or fried foods – Chocolate – Caffeine – Alcohol – Peppermint – Lying down soon after eating – especially large meals – Obesity and pregnancy (which increase abdominal pressure). These are lifestyle-related and often reproducible; a person with GERD can usually pinpoint specific dietary choices or habits that exacerbate their symptoms. The timing of symptoms is also important. They tend to occur shortly after eating, during or after exercise, or when lying down.
Panic attacks, on the other hand, are frequently triggered by stress, anxiety-provoking situations, or even seemingly innocuous events that evoke a sense of threat. These triggers can be internal (worrisome thoughts) or external (a stressful work environment). However, many panic attacks occur unexpectedly, without any identifiable trigger—a phenomenon known as spontaneous panic attacks. The symptoms typically peak within minutes and then gradually subside. Unlike GERD, where discomfort may persist for hours, a panic attack usually lasts only 10-20 minutes. This rapid onset and offset are distinguishing features. Planning ahead can reduce stress – perhaps by learning how to plan a gut friendly weekend.
It’s essential to recognize that these conditions can interact with each other. Chronic GERD can lead to anxiety about experiencing symptoms, potentially triggering panic attacks. Conversely, the hyperventilation associated with panic attacks can actually worsen GERD symptoms by increasing abdominal pressure and promoting reflux. This creates a challenging cycle where it’s difficult to discern which condition is primary or secondary.
Diving Deeper: Symptom Specificity
Chest Pain Characteristics
As previously mentioned, the quality of chest pain differs between GERD and panic attacks. GERD-related chest pain is typically described as burning, squeezing, or pressure in the mid-chest area. It’s often mistaken for heart attack pain because it can radiate to the jaw, neck, or back. However, unlike cardiac chest pain which is often brought on by exertion, GERD pain is more likely to occur after meals or when reclining. A crucial question to ask yourself (and relay to your doctor) is: “Does this pain feel like someone is sitting on my chest, or does it burn from the inside?”
Panic attack chest pain tends to be sharper, stabbing, and can be located anywhere in the chest – not necessarily behind the breastbone. It’s often accompanied by a feeling of tightness or constriction. Importantly, panic attack-related chest pain usually doesn’t respond to antacids or acid-reducing medications, whereas GERD pain often does. A key indicator is whether over-the-counter remedies for heartburn provide any relief. If the pain persists despite these measures, it’s less likely to be GERD.
Breathing Difficulties & Associated Sensations
Both conditions can cause shortness of breath or difficulty breathing, but the underlying mechanisms are different. In GERD, breathing difficulties may stem from acid reflux irritating the airways, leading to a chronic cough or asthma-like symptoms. The sensation is often described as tightness in the chest making it hard to take a deep breath. However, it’s usually accompanied by other GERD symptoms like heartburn and acid regurgitation.
Panic attacks cause rapid, shallow breathing (hyperventilation) due to the activation of the fight-or-flight response. This can lead to dizziness, lightheadedness, and tingling sensations in the extremities. The individual may feel as though they are suffocating or unable to get enough air—a terrifying sensation that drives further anxiety. This hyperventilation is a physical manifestation of intense fear, not a symptom of digestive distress.
Psychological Components & Accompanying Feelings
Panic attacks are characterized by an overwhelming sense of fear, dread, and impending doom. Individuals often report feeling detached from reality or experiencing a loss of control. These psychological components are absent in GERD, which primarily involves physical symptoms. While chronic GERD can lead to anxiety and stress due to its disruptive nature, it doesn’t trigger the acute, intense fear associated with panic attacks.
A helpful question to consider is: “Am I afraid that I’m dying or losing control?” If the answer is yes, a panic attack is more likely. Conversely, if the primary concern is discomfort and digestive symptoms, GERD is a stronger possibility. However, it’s important to remember that anxiety can mimic many physical sensations, making accurate self-assessment challenging. Learning [how to build a minimal ingredient meal plan] can remove stress from food choices.
It’s crucial to reiterate that this information is for educational purposes only and should not be used as a substitute for professional medical advice. If you are experiencing chest pain or difficulty breathing, seek immediate medical attention. A healthcare provider can perform a thorough evaluation to determine the cause of your symptoms and recommend appropriate treatment. They may utilize diagnostic tests such as an endoscopy for GERD assessment or an electrocardiogram (ECG) to rule out cardiac issues. Early diagnosis and proper management are essential for both GERD and panic attacks, improving quality of life and preventing complications. You could also consider [how to recover after a digestive flare up] if symptoms persist.