Gastroesophageal reflux disease (GERD) and chronic hiccups – seemingly disparate conditions – can surprisingly intertwine, creating a frustrating cycle for those affected. GERD, characterized by frequent acid reflux, is a common digestive disorder impacting millions globally. Chronic hiccups, defined as persistent hiccups lasting longer than 48 hours, are far less prevalent but equally disruptive to daily life. While often dismissed as a temporary annoyance, chronic hiccups can significantly impair quality of life, leading to exhaustion, difficulty eating, and even social isolation. Understanding the potential link between these two conditions is crucial for effective diagnosis and management, moving beyond simple remedies toward addressing underlying causes.
The connection isn’t always immediately obvious, because the mechanisms are complex and often involve a bidirectional relationship: GERD can trigger hiccups, but persistent hiccups themselves might exacerbate or even contribute to GERD symptoms. This interplay is rooted in shared neurological pathways and anatomical proximity between the esophagus and the diaphragm – the primary muscle involved in both breathing (and thus hiccuping) and esophageal function. Recognizing this connection allows healthcare professionals to consider a more holistic approach to patient care, looking beyond surface-level treatments for long-term relief. The following will delve into the intricacies of this relationship, exploring how GERD can contribute to chronic hiccups, the potential mechanisms involved, and strategies for managing both conditions effectively.
The Role of GERD in Triggering Chronic Hiccups
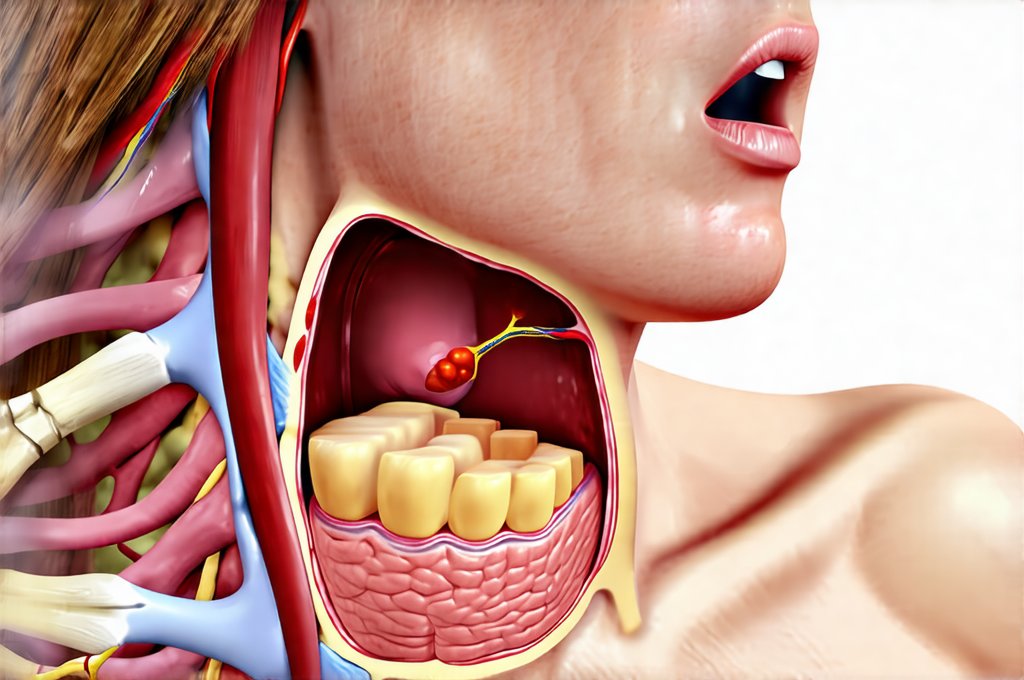
The link between GERD and hiccups stems from the irritation and inflammation caused by frequent acid reflux. When stomach acid repeatedly flows back into the esophagus, it doesn’t just irritate the esophageal lining; it can also stimulate the vagus nerve. This long cranial nerve runs from the brainstem down to the abdomen, playing a vital role in controlling numerous bodily functions including digestion, heart rate, and – crucially for our discussion – the diaphragm. Acid reflux-induced irritation of the esophagus activates receptors along the vagus nerve, sending signals that can inadvertently trigger hiccup reflexes. This is often described as a reflex arc gone awry, where the normal signaling pathways become overstimulated.
Furthermore, GERD can lead to esophagitis, or inflammation of the esophagus. The persistent inflammation not only increases vagal nerve stimulation but also impacts esophageal motility – how efficiently food moves down the digestive tract. Disruptions in motility can alter pressure dynamics within the chest and abdomen, potentially contributing to diaphragmatic spasms that manifest as hiccups. It’s important to understand this isn’t a direct cause-and-effect relationship for everyone with GERD; many experience reflux without developing chronic hiccups. However, individuals prone to more severe or frequent reflux episodes are statistically more likely to experience hiccup issues.
The type of food and drink consumed can also play a significant role here. Foods known to trigger GERD – such as spicy foods, caffeine, alcohol, fatty meals, and chocolate – indirectly increase the likelihood of hiccups in susceptible individuals by intensifying reflux symptoms and vagal nerve stimulation. This highlights why dietary modifications are often crucial components of managing both conditions simultaneously. In essence, reducing acid production and minimizing esophageal irritation through lifestyle changes can be a proactive step toward preventing hiccup episodes triggered by GERD.
Understanding the Vagus Nerve Connection
The vagus nerve is central to understanding this complex relationship. It’s not simply a conduit for triggering hiccups; it’s an intricate communication network that connects the gut and brain – often referred to as the “gut-brain axis”. When acid reflux occurs, sensory receptors in the esophagus detect the irritation and send signals along the vagus nerve to the brainstem. The brainstem then attempts to regulate the situation, sometimes resulting in inappropriate or overactive reflexes, including hiccuping. This is because the same neural pathways involved in normal digestive function are also implicated in hiccup generation.
The sensitivity of the vagus nerve can vary significantly between individuals. Some people have a higher threshold for irritation and may experience reflux without triggering hiccups, while others are more sensitive and prone to developing them even with mild reflux episodes. This variability explains why not everyone with GERD experiences chronic hiccups. Moreover, conditions that affect vagal tone – such as stress, anxiety, or certain medications – can further exacerbate the issue, making individuals more susceptible to hiccup triggers.
- Vagal nerve stimulation is also used therapeutically for some medical conditions (e.g., epilepsy), demonstrating its powerful influence on neurological function. This highlights how easily this system can be disrupted and lead to unwanted reflexes like hiccups.
- The brainstem’s interpretation of vagal signals is crucial. Misinterpretation or overstimulation can result in the initiation of hiccuping even when there isn’t a genuine physiological need for it.
Hiccups Exacerbating GERD: A Vicious Cycle
While GERD can cause hiccups, chronic hiccups themselves can also worsen GERD symptoms, creating a frustrating and self-perpetuating cycle. The forceful contractions of the diaphragm during hiccuping create significant pressure changes within the abdomen and chest. These pressure fluctuations can disrupt the lower esophageal sphincter (LES), the muscular valve that prevents stomach acid from flowing back into the esophagus. When the LES is compromised, it allows more acid to reflux, further irritating the esophagus and stimulating the vagus nerve – thus potentially triggering more hiccups.
This bidirectional relationship makes diagnosis and treatment challenging. Patients may initially seek help for hiccups only to discover underlying GERD contributing to their symptoms. Conversely, individuals with chronic GERD may find their reflux worsens after experiencing prolonged bouts of hiccups. The pressure changes also affect esophageal motility, further disrupting the digestive process and potentially leading to more frequent or severe acid reflux episodes.
The constant cycle can lead to increased inflammation and damage to the esophageal lining over time. This not only exacerbates GERD symptoms but can also increase the risk of complications like Barrett’s esophagus – a precancerous condition. It’s crucial to break this vicious cycle through comprehensive management strategies addressing both conditions simultaneously, rather than treating them in isolation.
Diagnostic Approaches and Management Strategies
Diagnosing the connection between GERD and chronic hiccups often requires a careful evaluation of symptoms and medical history. Doctors may use several tools including:
1. Endoscopy: A procedure where a thin, flexible tube with a camera is inserted into the esophagus to visualize any inflammation or damage.
2. Esophageal manometry: Measures the pressure within the esophagus to assess esophageal motility and LES function.
3. pH monitoring: Determines the amount of acid reflux occurring over a 24-hour period.
Management strategies should be tailored to the individual patient, addressing both GERD and hiccups. For GERD, this typically involves:
– Lifestyle modifications such as dietary changes (avoiding trigger foods) and elevating the head of the bed.
– Over-the-counter medications like antacids or H2 blockers.
– Prescription proton pump inhibitors (PPIs) to reduce acid production in more severe cases.
For chronic hiccups, initial approaches may include:
– Simple remedies like drinking water rapidly or holding your breath (though these are often ineffective for persistent hiccups).
– Medications such as baclofen or chlorpromazine, which can help suppress hiccup reflexes (prescribed by a doctor only).
– In rare cases, nerve blocks or surgical interventions may be considered.
The most important aspect is recognizing the connection and adopting a holistic treatment plan. This might involve working closely with a gastroenterologist and potentially a neurologist to optimize management of both conditions simultaneously. Cognitive behavioral therapy (CBT) can also be beneficial in managing stress and anxiety that may contribute to both GERD and hiccup frequency. Ultimately, successful management requires a proactive approach focused on identifying triggers, minimizing irritation, and restoring balance to the digestive system and nervous system. If you experience frequent heartburn or acid reflux, understanding the connection between GERD and nausea can help manage your symptoms. Furthermore, exploring are gums and thickeners bad for the gut might reveal hidden triggers contributing to digestive discomfort. Many find relief by understanding the connection between GERD and throat clearing. Additionally, consider if are sweeteners the cause of chronic gas contributes to your digestive issues. For some, understanding GERD and sleep apnea: exploring the connection is vital for comprehensive care, and finally, don’t dismiss the connection between GERD and hiccups.