Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide. Most people experience occasional heartburn, but for those with GERD, this becomes frequent enough to significantly impact quality of life. Symptoms range from mild discomfort to severe pain and can include regurgitation, difficulty swallowing, and even chronic cough. Traditional understanding of GERD focuses on factors like lower esophageal sphincter (LES) dysfunction, hiatal hernia, and dietary influences—but increasingly, research is pointing towards a more nuanced picture that includes the role of the vagus nerve. This often-overlooked cranial nerve plays a critical part in gut-brain communication and overall digestive health.
The conventional approach to GERD largely centers on reducing stomach acid production with medications like proton pump inhibitors (PPIs) or addressing LES issues. While these treatments can be effective for many, they don’t always provide long-term solutions and can sometimes have unwanted side effects. This is prompting a deeper exploration of the underlying mechanisms driving GERD, leading to growing interest in the connection between the vagus nerve and digestive health. Understanding this relationship could unlock new avenues for managing and potentially alleviating symptoms – shifting focus from solely suppressing acid to supporting the body’s natural regulatory systems.
The Vagus Nerve: A Master Regulator of Digestion
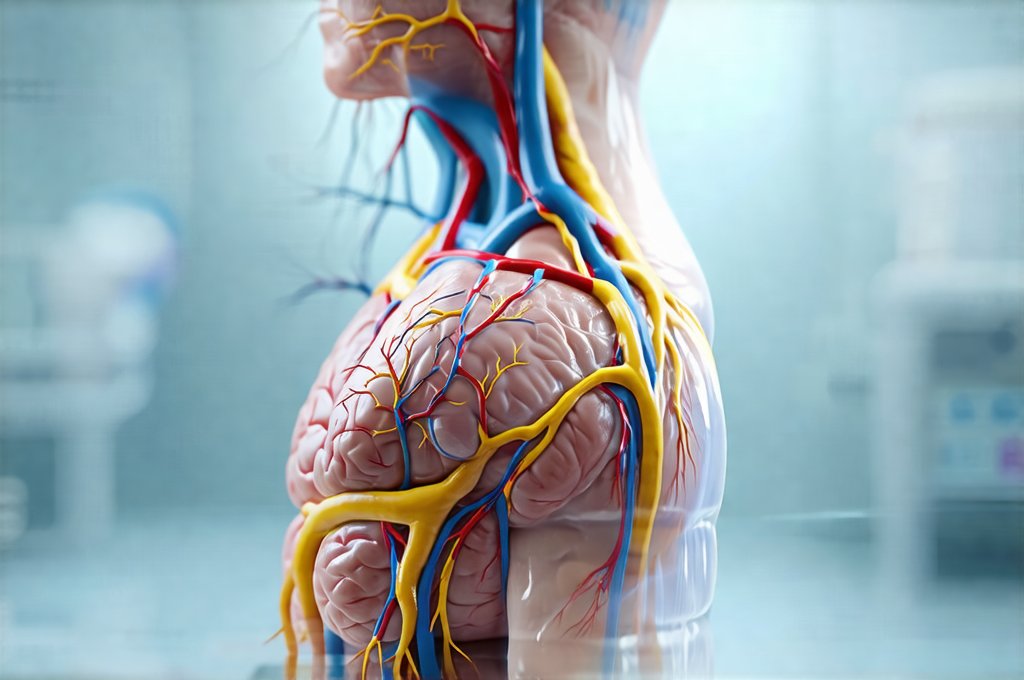
The vagus nerve isn’t just one nerve; it’s actually a pair of cranial nerves extending from the brainstem down through the neck and into the abdomen, branching out to connect with major organs including the heart, lungs, stomach, and intestines. It is often referred to as the tenth cranial nerve (CN X). Its name, derived from the Latin word for “wandering,” aptly describes its extensive reach throughout the body. Its primary function is to manage the parasympathetic nervous system – often dubbed the “rest and digest” system – which counteracts the “fight or flight” response of the sympathetic nervous system.
The vagus nerve’s influence on digestion is profound. It controls: – Gastric motility (the movement of food through the digestive tract) – Stomach acid production – Pancreatic enzyme secretion – Bile release from the gallbladder – Intestinal peristalsis (wave-like contractions that move waste along) Essentially, it regulates almost every step of the digestive process. A healthy vagus nerve ensures efficient digestion and nutrient absorption, while vagal dysfunction can contribute to a wide range of gastrointestinal issues, potentially including GERD.
A key aspect of vagal function is its bidirectional communication. It’s not just sending signals from the brain to the gut; it’s also relaying information from the gut back to the brain. This “gut-brain axis” allows for constant feedback and regulation, ensuring that digestive processes are aligned with the body’s overall needs. When this communication is disrupted – perhaps due to stress, inflammation, or other factors – it can lead to imbalances in digestion and contribute to symptoms like heartburn and reflux.
Vagal Tone and GERD Symptoms
Vagal tone refers to the level of activity within the vagus nerve. Higher vagal tone generally indicates better parasympathetic nervous system function and is associated with improved digestive health, reduced inflammation, and greater resilience to stress. Conversely, low vagal tone can manifest as digestive issues like bloating, constipation, diarrhea, and – importantly – increased susceptibility to GERD. Research suggests that individuals with lower vagal tone may experience more frequent and severe GERD symptoms.
The link between low vagal tone and GERD isn’t fully understood but several theories exist. One is that reduced vagal stimulation can lead to delayed gastric emptying, meaning food stays in the stomach for longer periods. This increases pressure within the stomach, potentially forcing acid up into the esophagus – a primary cause of heartburn. Another theory proposes that low vagal tone might weaken LES function, making it easier for acid to reflux. It’s likely a combination of these factors, along with impaired gut motility and increased inflammation, contributing to the problem.
Improving vagal tone is becoming an increasingly popular approach to managing digestive disorders, including GERD. This can be achieved through various lifestyle interventions that stimulate the vagus nerve – things like deep diaphragmatic breathing exercises, meditation, cold water immersion, singing, gargling, and even probiotics to support gut health (as a healthy gut promotes vagal signaling). These methods aim to “tone” the vagus nerve, strengthening its connection between the brain and the digestive system.
The Role of Inflammation and Gut Microbiome
Chronic inflammation is a significant driver of both GERD and vagal dysfunction. When the body is in a state of chronic inflammation – often triggered by diet, stress, or underlying health conditions – it can impair vagus nerve signaling, reducing its ability to effectively regulate digestion. Inflammatory molecules can also directly damage vagal fibers, further compromising their function. This creates a vicious cycle where inflammation worsens GERD symptoms and impaired vagal tone exacerbates inflammation.
The gut microbiome—the trillions of bacteria residing in our digestive tract—plays a crucial role in modulating inflammation and influencing vagal nerve activity. A healthy, diverse gut microbiome promotes anti-inflammatory signals and supports optimal vagal function. However, imbalances in the gut microbiome (dysbiosis) can lead to increased intestinal permeability (“leaky gut”), allowing inflammatory substances to enter the bloodstream. This triggers systemic inflammation and disrupts vagal signaling.
Diet plays a significant role here. A diet high in processed foods, sugar, and unhealthy fats can contribute to dysbiosis and inflammation, while a diet rich in fiber, prebiotics (foods that feed beneficial bacteria), and probiotics (live microorganisms) supports a healthy gut microbiome and promotes optimal vagal function. Addressing gut health through dietary changes and targeted supplementation can be an important component of managing GERD alongside other interventions. Understanding gut health is key to overall wellness.
Stimulating the Vagus Nerve for Relief
Fortunately, there are several practical strategies to stimulate the vagus nerve and potentially alleviate GERD symptoms. These methods are generally safe, accessible, and can be incorporated into daily routines. It’s worth noting that these approaches aren’t a quick fix; consistency is key. The goal is to gradually increase vagal tone over time.
- Diaphragmatic Breathing: Deep, slow breathing exercises activate the vagus nerve by stimulating the diaphragm – a major muscle involved in respiration and connected to the vagus nerve. Practicing 5-10 minutes of diaphragmatic breathing several times a day can be incredibly beneficial.
- Cold Water Immersion/Splashing: Brief exposure to cold water, such as splashing your face with cold water or taking a cold shower, stimulates the vagus nerve. Start slowly and gradually increase the duration and intensity.
- Gargling: Actively gargling for 30-60 seconds can stimulate the muscles in the throat that are innervated by the vagus nerve. Use water or even salt water for added benefits.
- Singing/Humming: Vocalizing, whether singing, humming, or chanting, activates the vagus nerve and promotes relaxation.
- Probiotics & Prebiotics: Supporting a healthy gut microbiome with probiotic-rich foods (yogurt, kefir, sauerkraut) and prebiotic-rich foods (garlic, onions, bananas) can enhance vagal signaling. Considering best time to take probiotics can also be helpful.
It’s important to remember that GERD is complex. While the vagus nerve plays a significant role, it’s rarely the sole factor involved. A holistic approach – addressing diet, stress levels, gut health, and lifestyle factors – is often necessary for long-term relief. If you are experiencing persistent or severe GERD symptoms, it’s essential to consult with a healthcare professional for proper diagnosis and treatment. Additionally, understanding GERD and asthma can provide further insight into related health concerns. Lastly, the connection between GERD and hiccups is a common concern for many patients, as well as the connection to throat clearing.