Gastroesophageal reflux disease (GERD), commonly experienced as heartburn, is often perceived as a digestive issue. However, its reach extends far beyond the esophagus, impacting seemingly unrelated areas of the body—one particularly intriguing connection being chronic sinus infections, also known as chronic rhinosinusitis. Many individuals suffering from persistent sinus problems may not realize that the root cause could be linked to stomach acid traveling upwards. This article will delve into the complex relationship between GERD and chronic sinusitis, exploring how reflux can contribute to inflammation in the sinuses, why some people are more susceptible than others, and what steps you can take to manage both conditions effectively. Understanding this connection is crucial for achieving long-term relief from these frustrating health concerns.
The prevalence of both GERD and chronic sinus infections is significant, making this interplay a common yet often overlooked issue. While occasional heartburn is normal, frequent or severe symptoms signal GERD. Similarly, acute sinus infections are typically caused by viruses and resolve within a few weeks. However, when sinusitis becomes chronic, defined as lasting 12 weeks or longer, the underlying cause is frequently more complex—and reflux can be a significant contributing factor. Recognizing this connection allows for a more targeted approach to treatment, moving beyond simply addressing sinus symptoms and tackling the potential source of inflammation. This article aims to provide you with a comprehensive overview of this relationship, empowering you to discuss it with your healthcare provider and explore appropriate management strategies.
The Mechanisms Linking GERD and Sinusitis
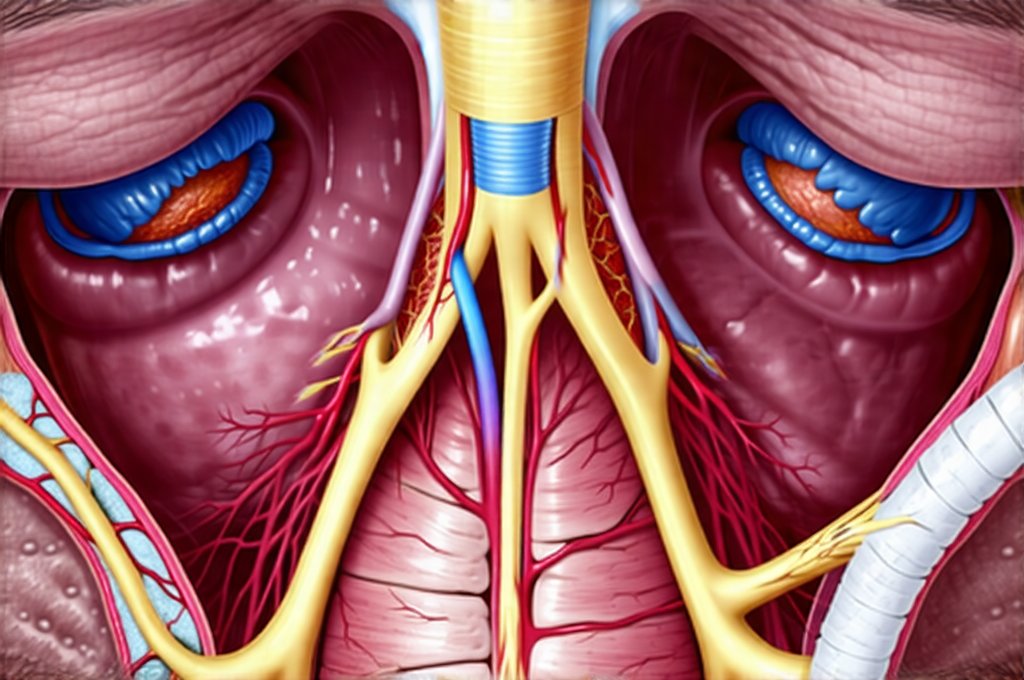
The connection between GERD and chronic sinusitis isn’t as straightforward as simply stomach acid directly irritating the sinuses. Instead, it’s a more nuanced interplay involving multiple factors. One primary mechanism is microaspiration, where small amounts of refluxed material—including stomach acid, pepsin (a digestive enzyme), and bile acids—travel up into the esophagus, then potentially into the back of the throat and even the nasal passages. This isn’t typically felt as heartburn; it’s a silent ascent that can occur during sleep or while lying down. While the amount is small, over time, these repeated microaspirations contribute to chronic inflammation in the sinuses.
Furthermore, reflux can trigger an inflammatory response systemically. The body recognizes stomach acid where it shouldn’t be and initiates an immune reaction. This systemic inflammation doesn’t just affect the esophagus; it can impact various tissues throughout the body, including those lining the nasal passages and sinuses. This ongoing inflammatory state makes individuals more susceptible to both bacterial and fungal sinus infections, and impairs the natural clearance mechanisms of the sinuses—the cilia that sweep mucus and debris out. The result is a vicious cycle: reflux contributes to inflammation, which hinders sinus drainage, leading to infection, further exacerbating the initial problem.
Finally, it’s important to understand the role of pepsin. While stomach acid gets most of the attention, pepsin is often more damaging to the upper airway and sinuses. Pepsin continues to break down proteins even in a neutral or slightly alkaline environment, meaning it can remain active long after the acid has been neutralized. This persistent enzymatic activity contributes significantly to inflammation and tissue damage within the sinus cavities. This explains why some individuals with reflux experience significant sinusitis despite not having particularly high levels of stomach acidity. Understanding the link between liver health can further help to address related inflammation.
Understanding Laryngopharyngeal Reflux (LPR)
A key component in this connection is often laryngopharyngeal reflux (LPR), sometimes referred to as “silent reflux.” Unlike typical GERD, which presents with classic heartburn symptoms, LPR frequently lacks these obvious indicators. Instead, it manifests with a variety of more subtle—and often misinterpreted—symptoms like chronic cough, hoarseness, throat clearing, and a sensation of something stuck in the back of the throat (globus sensation). These are all signs that refluxed material is reaching the larynx (voice box) and pharynx (throat), creating irritation and inflammation.
LPR is particularly relevant to sinus issues because the proximity of the upper airway allows for easy access of refluxed material to the nasal passages. Even small amounts of acid or pepsin can irritate the delicate tissues lining these areas, leading to chronic sinusitis. It’s important to note that many people with LPR don’t experience typical heartburn symptoms, making diagnosis challenging. Standard GERD tests may not always be sufficient to detect LPR; specialized testing, such as impedance-pH monitoring, is often required for accurate assessment. Experiencing issues like this can also reveal gut pain and emotional triggers.
The Role of Nasal Congestion and Eustachian Tube Dysfunction
Nasal congestion, a hallmark symptom of sinusitis, can actually worsen reflux symptoms—creating another layer of complexity in this relationship. When nasal passages are blocked, it increases negative pressure within the chest cavity, making it easier for stomach acid to flow back up into the esophagus. This creates a feedback loop: reflux causes sinus inflammation and congestion, which then exacerbates reflux, leading to even more sinus problems.
Adding to this complexity is Eustachian tube dysfunction. The Eustachian tubes connect the middle ear to the back of the throat, helping to equalize pressure and drain fluids. When these tubes are blocked or malfunctioning—often due to inflammation from sinusitis—it can lead to fluid buildup in the ears, hearing loss, and a feeling of fullness in the ears. Reflux can also directly irritate the Eustachian tubes, contributing to their dysfunction. This interplay between reflux, sinus congestion, and Eustachian tube problems creates a cascade of symptoms that can significantly impact quality of life. Understanding food reactions is also important when considering inflammation.
Identifying Risk Factors and Diagnostic Approaches
Certain individuals are more predisposed to developing both GERD and chronic sinusitis. These risk factors include: – Obesity – Excess weight puts pressure on the abdomen, increasing the likelihood of reflux. – Hiatal hernia – A condition where part of the stomach protrudes through the diaphragm, weakening the barrier between the esophagus and stomach. – Smoking – Damages the esophageal sphincter, allowing acid to flow back more easily. – Certain foods – Fatty or fried foods, chocolate, caffeine, and alcohol can all trigger reflux. – Pregnancy – Hormonal changes and increased abdominal pressure during pregnancy can increase risk.
Diagnosing the connection requires a comprehensive approach. A thorough medical history, including detailed information about both GERD and sinus symptoms, is crucial. Physical examination of the nose and throat allows for assessment of inflammation and congestion. Diagnostic tests may include: 1. Endoscopy – To visualize the esophagus and stomach for signs of reflux damage. 2. Impedance-pH monitoring – A more sensitive test to detect LPR, even in the absence of heartburn symptoms. 3. Sinus CT scan – To evaluate the extent of sinus inflammation and rule out other causes of chronic sinusitis, such as nasal polyps or structural abnormalities. 4. Allergy testing – To identify potential allergic triggers that may be contributing to sinus inflammation. Exploring the link between gut pain and additives can also help with diagnosis.
It’s essential to remember that self-diagnosing is not advisable. A healthcare professional can accurately assess your symptoms, determine the underlying cause, and recommend an appropriate treatment plan tailored to your individual needs. The goal isn’t simply to treat the symptoms of either GERD or sinusitis in isolation but to address the interconnectedness of these conditions for lasting relief. Sometimes perfectionism can exacerbate stress and related health issues. Also, consider that seafood may contribute to digestive discomfort in some individuals.